The procedure for organizing and monitoring the volumes, terms, quality and conditions for the provision of medical care for compulsory medical insurance - Rossiyskaya Gazeta. Control of volumes, terms, quality and conditions for the provision of medical care
"Issues of expertise and quality of medical care", 2013, N 3
What document should be used when organizing control of the volume and quality of medical care under compulsory medical insurance?
Answer. The main regulatory document in this area is the FFOMS order dated 01.12.2010 N 230 (as amended on 16.08.2011) "On approval of the Procedure for organizing and monitoring the volume, timing, quality and conditions of providing medical care under compulsory medical insurance". The order defines the rules and procedure for organizing and conducting by medical insurance organizations and CHI funds control over the volumes, terms, quality and conditions for the provision of medical care by medical organizations in the amount and on the terms established by the territorial CHI program and the agreement for the provision and payment of medical care under CHI. It should be borne in mind that in many constituent entities of the Russian Federation, on the basis of this document, their own similar regional orders and methodological recommendations were developed and approved.
What is meant by the control of volumes, terms, quality and conditions for the provision of medical care under compulsory medical insurance?
Answer. The control of the volume, timing, quality and conditions for the provision of medical care under compulsory medical insurance (hereinafter - control) includes measures to verify the compliance of the medical care provided to the insured with the terms of the contract for the provision and payment of medical care under compulsory medical insurance, implemented through medical and economic control, medical and economic examination and examination of the quality of medical care (KMP). The object of control is the organization and provision of medical care under compulsory medical insurance. The subjects of control are territorial CHI funds, medical insurance organizations, medical organizations entitled to carry out medical activities and are included in the register of medical organizations operating in compulsory health insurance.
What are the main goals of control?
Answer. The main objectives of control are:
- ensuring free provision of medical care to the insured person in the amount and under the conditions established by the territorial CHI program;
- protection of the rights of the insured person to receive free medical care in the amount and under the conditions established by the territorial CHI program, of proper quality in medical organizations participating in the implementation of CHI programs, in accordance with contracts for the provision and payment of medical care under CHI;
- prevention of medical care defects resulting from the inadequacy of the medical care provided to the health state of the insured person; non-compliance and / or incorrect implementation of the procedures for the provision of medical care and / or standards of medical care, medical technologies by analyzing the most common violations based on the results of control and taking measures by the authorized bodies;
- verification of the fulfillment by medical insurance organizations and medical organizations of obligations to pay and provide free medical care to insured persons under compulsory medical insurance programs;
- verification of the fulfillment of obligations by medical insurance organizations to study the satisfaction of insured persons with the volume, availability and quality of medical care;
- optimization of the cost of paying for medical care in the event of an insured event and reduction of insurance risks in compulsory health insurance.
What is meant by medical and economic control?
Answer. Under medical and economic control in accordance with part 3 of article 40 of the Federal Law of 29.11.2010 N 326-FZ "On compulsory health insurance in Russian Federation"(hereinafter - the Federal Law) means the establishment of compliance of information on the volume of medical care provided to insured persons on the basis of the registers of accounts provided for payment by the medical organization to the terms of contracts for the provision and payment of medical care under the CHI territorial CHI program, methods of payment for medical care and tariffs for payment of medical Medical and economic control is carried out by specialists of medical insurance organizations and territorial CHI funds.
During medical and economic control, all cases of medical care under compulsory medical insurance are monitored in order to:
- checking account registers for compliance with the established procedure for information exchange in the field of CHI;
- identification of the person insured by a specific medical insurance organization (payer);
- checking the compliance of the medical care provided: a) the territorial compulsory medical insurance program; b) the terms of the contract for the provision and payment of medical care under compulsory medical insurance; c) a valid license medical organization to carry out medical activities;
- checking the validity of the application of tariffs for medical services, calculating their cost in accordance with the methodology for calculating tariffs for payment for medical care approved by the authorized federal executive body, methods of payment for medical care and tariffs for paying for medical care and an agreement for the provision and payment of medical care under compulsory medical insurance;
- establishing that the medical organization does not exceed the volume of medical care established by the decision of the commission for the development of territorial program CHI payable by compulsory medical insurance funds.
The violations identified in the registers of accounts are reflected in the act of medical and economic control with an indication of the amount of reduction of the bill for each register entry containing information about defects in medical care and / or violations in the provision of medical care. In accordance with parts 9 and 10 of Article 40 of the Federal Law, the results of medical and economic control drawn up by the relevant act are the basis for the application of the measures provided for in Article 41 of the Federal Law, the terms of the contract for the provision and payment of medical care under compulsory medical insurance and the list of grounds for refusing to pay for medical assistance (reduction of payment for medical care), and may also be the basis for a medical and economic examination; organizing and conducting an examination of the ILC; repeated medical and economic control, repeated medical and economic examination and examination of the ILC by the territorial CHI fund or by an insurance medical organization on the instructions of the territorial fund (except for control when making payments for medical care provided to insured persons outside the constituent entity of the Russian Federation, on the territory of which the policy was issued OMS).
What is meant by medical and economic expertise?
Answer. Medical and economic examination in accordance with Part 4 of Article 40 of the Federal Law - establishing the correspondence between the actual terms of medical care, the amount presented for payment medical services records in primary medical documentation and accounting and reporting documentation of a medical organization. Medical and economic expertise is carried out in the form of: a) targeted medical and economic expertise; b) planned medical and economic examination.
Targeted medical and economic examination is carried out in the following cases:
a) repeated visits for the same disease: within 30 days - in the provision of outpatient care, within 90 days - in case of repeated hospitalization;
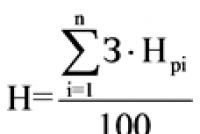
b) diseases with an extended or shortened period of treatment by more than 50 percent of the established standard of medical care or average for all insured persons in reporting period with a disease for which there is no approved standard of care;
c) receiving complaints from the insured person or his representative about the availability of medical care in a medical organization.
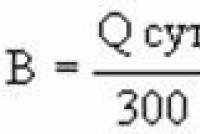
On the basis of the conducted medical and economic control, a planned medical and economic examination is carried out according to invoices submitted for payment within a month after the provision of medical assistance to the insured person under compulsory medical insurance, in other cases it can be carried out within a year after the presentation of invoices for payment.
When carrying out a planned medical and economic examination, the following are assessed:
a) the nature, frequency and reasons of violations of the rights of insured persons to receive medical care under the CHI in the amount, terms, quality and conditions established by the contract for the provision and payment of medical care under the CHI;
b) the volume of medical care provided by the medical organization and its compliance with the amount established by the decision of the commission for the development of the territorial CHI program to be paid from the CHI funds;
c) the frequency and nature of violations by a medical organization of the procedure for forming account registers.
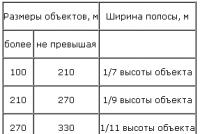
The volume of monthly planned medical and economic examinations from the number of bills accepted for payment in cases of medical care under compulsory medical insurance is determined by the plan of inspections by medical insurance organizations of medical organizations, agreed by the territorial compulsory medical insurance fund, and is at least:
8% - inpatient medical care;
8% - medical care provided in the day hospital;
0.8% - outpatient and polyclinic medical care.
If within a month the number of defects in medical care and / or violations in the provision of medical care exceeds 30 percent of the number of cases of medical care for which a medical and economic examination was carried out, in the next month the volume of checks from the number of bills accepted for payment in cases the provision of medical assistance should be increased by at least 2 times compared to the previous month.
For a certain set of cases of medical care, selected according to thematic criteria (for example, the frequency and types of postoperative complications, duration of treatment, cost of medical services) in a medical organization, in accordance with the plan agreed by the territorial CHI fund, a planned thematic medical and economic examination can be carried out ...
Based on the results of the medical and economic examination, the expert expert draws up an act of the medical and economic examination in two copies: one is transferred to the medical organization, one copy remains in the medical insurance organization / territorial CHI fund.
In accordance with part 9 of Article 40 of the Federal Law, the results of a medical and economic examination, drawn up by an appropriate act in the form established by the Federal CHI Fund, are the basis for the application of measures to a medical organization provided for in Article 41 of the Federal Law, the terms of an agreement for the provision and payment of medical care for Compulsory medical insurance and a list of grounds for refusing to pay for medical care (reducing the payment for medical care), and may also be the basis for an examination of the ILC.
What is meant by the expertise of the ILC?
Answer. In accordance with Part 6 of Article 40 of the Federal Law, the examination of the ILC is the identification of violations in the provision of medical care, including the assessment of the correctness of the choice of medical technology, the degree of achievement of the planned result and the establishment of cause-and-effect relationships of the identified defects in the provision of medical care.
The examination of the ILC is carried out by checking the compliance of the medical care provided to the insured person with the contract for the provision and payment of medical care under the compulsory medical insurance, the procedures for the provision of medical care and the standards of medical care, established clinical practice.
The examination of the ILC is carried out by an ILC expert, included in the territorial register of ILC experts on behalf of the territorial CHI fund or an insurance medical organization.
The examination of the ILC is carried out in the form of: a) targeted expertise of the ILC; b) planned examination of the ILC.
Targeted examination of the ILC is carried out in the following cases:
- receiving complaints from the insured person or his representative about the availability and quality of medical care in a medical organization;
- deaths in the provision of medical care;
- nosocomial infection and complications of the disease;
- primary disability for people of working age and children;
- repeated justified treatment for the same disease: within 30 days - when providing outpatient care, within 90 days - with repeated hospitalization;
- diseases with an extended or shortened treatment period by more than 50 percent of the established standard of medical care or the average for all insured persons in the reporting period with a disease for which there is no approved standard of medical care.
When conducting a targeted examination of the ILC in cases selected according to the results of a targeted medical and economic examination, the total time for conducting a targeted examination of the ILC may increase up to six months from the date of the invoice for payment.
When conducting a targeted examination of the ILC in cases of repeated admission (hospitalization) for the same disease deadlines are calculated from the moment of submission for payment of an invoice containing information on re-admission (hospitalization).
The timing of the targeted examination of the ILC from the moment the invoice is submitted for payment is not limited in cases of complaints from insured persons or their representatives, deaths, nosocomial infection and complications of diseases, primary disability of people of working age and children.
Conducting a targeted examination of the ILC in case of receipt of complaints from insured persons or their representatives does not depend on the time elapsed since the provision of medical care and is carried out in accordance with Federal Law of 02.05.2006 N 59-FZ "On the Procedure for Considering Appeals of Citizens of the Russian Federation" and others regulatory legal acts governing the work with citizens' appeals.
The planned examination of the ILC is carried out in order to assess the compliance of the volumes, terms, quality and conditions for the provision of medical care to groups of insured persons, divided by age, disease or group of diseases, the stage of medical care and other signs, the conditions stipulated by the contract for the provision and payment of medical care under compulsory medical insurance ... The volume of monthly planned examinations of the ILC is determined by the plan of inspections by medical insurance organizations of medical organizations and is not less than: in a hospital - 5% of the number of completed treatment cases; day hospital - 3% of the number of completed treatment cases; in the provision of outpatient care - 0.5% of the number of completed treatment cases based on the results of medical and economic control.
The planned examination of the ILC is carried out on cases of medical care under the compulsory medical insurance, selected: a) by the method of random sampling; b) for a thematically homogeneous set of cases.
A planned examination of the ILC by the method of random sampling is carried out to assess the nature, frequency and causes of violations of the rights of insured persons to timely receive medical care of the volume and quality established by the territorial compulsory medical insurance program, including those caused by improper implementation of medical technologies that led to a deterioration in the health of the insured person, additional risk consequences for his health, suboptimal expenditure of resources of a medical organization, dissatisfaction with medical care of insured persons.
A planned thematic examination of the ILC is carried out in relation to a certain set of cases of medical care under compulsory medical insurance, selected according to thematic characteristics in each medical organization or group of medical organizations providing medical care under compulsory medical insurance of the same type or in the same conditions.
The choice of the topic is based on the performance indicators of medical organizations, their structural divisions and profile areas of activity: a) hospital mortality, the frequency of postoperative complications, the primary disability rate of people of working age and children, the frequency of re-hospitalizations, the average duration of treatment, the cost of medical services, and others. indicators; b) the results of internal and departmental control of the ILC.
The planned thematic examination of the ILC is aimed at solving the following tasks: a) identifying, establishing the nature and causes of typical (repeated, systematic) errors in the treatment and diagnostic process; b) comparison of the ILC provided to groups of insured persons, divided by age, gender and other characteristics.
A planned examination of the ILC is carried out in each medical organization providing medical care under the compulsory medical insurance, at least once during a calendar year within the timeframes determined by the inspection plan.
The examination of the ILC can be carried out during the period of rendering medical assistance to the insured person (hereinafter - the full-time examination of the ILC), including at the request of the insured person or his representative. The main goal of the full-time examination of the ILC is to prevent and / or minimize the negative impact on the patient's health status of medical care defects.
The ILC expert, with the notification of the administration of the medical organization, can conduct a by-pass of the departments of the medical organization in order to control the conditions for the provision of medical care, prepare materials for an expert opinion, as well as consult the insured person.
When consulting, the applied insured person is informed about his state of health, the degree of compliance of the provided medical care with the procedures for the provision of medical care and standards of medical care, the contract for the provision and payment of medical care under compulsory medical insurance with an explanation of his rights in accordance with the legislation of the Russian Federation.
The ILC expert, who carried out the ILC examination, draws up an expert opinion containing a description of the conduct and the results of the ILC examination, on the basis of which the ILC examination certificate is drawn up.
In accordance with parts 9 and 10 of Article 40 of the Federal Law, the results of the examination of the ILC, drawn up by the relevant act in the form established by the Federal CHI Fund, are the basis for the application of measures to a medical organization provided for in Article 41 of the Federal Law, the terms of the contract for the provision and payment of medical care for Compulsory medical insurance and a list of grounds for refusing to pay for medical care (reducing the payment for medical care).
Based on the ILC examination certificates, the authorized bodies are taking measures to improve the ILC.
How does the territorial CHI fund supervise the activities of medical insurance organizations in the field of control over the quality of medical care?
Answer. Territorial fund The compulsory medical insurance, on the basis of part 11 of article 40 of the Federal Law, exercises control over the activities of medical insurance organizations by organizing control over the volumes, terms, quality and conditions for the provision of medical care, conducts medical and economic control, medical and economic examination, examination of the ILC, including repeated.
Repeated medical and economic examination or examination of the ILC (hereinafter referred to as the re-examination) - a medical and economic examination conducted by another expert-expert or another expert of the ILC in order to verify the validity and reliability of conclusions on previously accepted conclusions made by a specialist-expert or an expert of ILC, primarily who conducted a medical and economic examination or examination of the ILC.
The repeated examination of the ILC can be carried out in parallel or sequentially with the first by the same method, but by a different ILC expert.
The objectives of the re-examination are: a) verification of the validity and reliability of the conclusion of a specialist-expert or an expert of the ILC, who initially conducted the medical and economic examination or the ILC examination; b) control of the activities of individual experts / experts of the ILC.
Re-examination is carried out in the following cases:
a) conducting a documentary audit of the organization by the territorial CHI fund OMS insurance a medical organization;
b) identification of violations in the organization of control by the medical insurance organization;
c) groundlessness and / or unreliability of the conclusion of the ILC expert who carried out the ILC examination;
d) receipt of a claim from a medical organization that has not been settled with an insurance medical organization.
The territorial CHI fund notifies the medical insurance organization and the medical organization about the re-examination no later than 5 working days before the start of work.
To conduct a re-examination of the territorial CHI fund within 5 working days after receiving the relevant request, the medical insurance organization and the medical organization must provide:
an insurance medical organization - copies of acts of medical and economic control, medical and economic examination and examination of the ILC necessary for re-examination;
medical organization - medical, accounting and reporting and other documentation, if necessary, the results of internal and departmental control of the ILC, including that carried out by the health management body.
The number of cases subject to re-examination is determined by the number of reasons for their conduct, but not less than 10% of the number of all examinations for the corresponding period of time, including at least 30% of re-examinations of the ILC.
During a calendar year, all medical insurance organizations operating in the field of compulsory medical insurance should be subject to re-examination in cases of medical care in all medical organizations in proportion to the number of bills presented for payment.
The territorial CHI fund sends the results of the re-examination, drawn up by the act, to the insurance medical organization and the medical organization no later than 20 working days after the end of the inspection. An insurance medical organization and a medical organization are obliged to consider these acts within 20 working days from the date of their receipt.
An insurance medical organization and a medical organization, in the absence of agreement with the results of the re-examination, send a signed act with a protocol of disagreements to the territorial CHI fund no later than 10 working days from the date of receipt of the act.
The territorial CHI fund, within 30 working days from the date of receipt, considers the act with the protocol of disagreements with the involvement of interested parties.
In accordance with part 14 of Article 38 of the Federal Law, the territorial CHI fund, in the event of violations of contractual obligations by an insurance medical organization, when reimbursing it for medical care costs, reduces payments by the amount of identified violations or unfulfilled contractual obligations.
The list of sanctions for violations of contractual obligations is established by an agreement on financial support CHI, concluded between the territorial CHI fund and an insurance medical organization.
In accordance with this agreement, in case of violations in the activities of an insurance medical organization, the territorial CHI fund uses measures applied to an insurance medical organization in accordance with part 13 of Article 38 of the Federal Law and an agreement on financial support of CHI or recognizes measures applied by an insurance medical organization to a medical organization unreasonable.
The territorial CHI fund, upon detecting violations in the organization and conducting a medical and economic examination and / or examination of the ILC, sends a claim to an insurance medical organization, which contains information about the control over the activities of an insurance medical organization:
a) the name of the commission of the territorial CHI fund;
b) the date (period) of the inspection of the medical insurance organization;
c) the composition of the commission of the territorial CHI fund;
d) regulatory legal acts, which are the basis for monitoring the activities of an insurance medical organization for organizing and conducting control and the reasons for conducting control;
e) facts of improper fulfillment by the medical insurance organization of contractual obligations to organize and conduct control, indicating the acts of re-examination;
f) the measure of liability of the medical insurance organization for the violations identified;
g) attachments (copies of re-examination acts, etc.).
The claim is signed by the director of the territorial CHI fund.
The execution of the claim is carried out within 30 working days from the date of its receipt by the medical insurance organization, about which the territorial CHI fund is informed.
If the territorial CHI fund reveals during the re-examination of violations missed by the medical insurance organization in the course of the medical and economic examination or the examination of the ILC, the medical insurance organization loses the right to use the measures applied to the medical organization for a timely undetected medical care defect and / or the provision of medical care.
The funds in the amount determined by the re-examination act are returned by the medical organization to the budget of the territorial CHI fund. Sanctions are applied to the medical insurance organization in accordance with the contract on financial support of the compulsory medical insurance.
The territorial CHI fund analyzes the applications of insured persons, their representatives and others cHI subjects based on the results of control carried out by an insurance medical organization.
How is the interaction of the subjects of control organized?
Answer. The territorial CHI fund coordinates the interaction of subjects of control on the territory of a constituent entity of the Russian Federation, conducts organizational and methodological work to ensure the functioning of control and protection of the rights of insured persons, coordinates the plans for the activities of medical insurance organizations in terms of organizing and conducting control, including plans for inspections by medical insurance organizations medical organizations providing medical care under contracts for the provision and payment of medical care under compulsory medical insurance.
When conducting a medical and economic examination and examination of the ILC, a medical organization provides specialists-experts and experts of the ILC within 5 working days after receiving a request, medical, accounting and reporting and other documentation, if necessary, the results of internal and departmental control of the ILC.
In accordance with part 8 of Article 40 of the Federal Law, a medical organization does not have the right to interfere with the access of specialist experts and experts of the ILC to the materials necessary for conducting a medical and economic examination, an examination of the ILC and is obliged to provide the requested information.
Employees participating in the control are responsible for the disclosure of confidential information of limited access in accordance with the legislation of the Russian Federation.
On the basis of Article 42 of the Federal Law, the resolution of controversial and conflict issues arising in the course of control between a medical organization and an insurance medical organization is carried out by the territorial CHI fund.
The commission informs the interested parties and the executive authority of the constituent entity of the Russian Federation in the field of healthcare on the results of resolving controversial and conflict issues, on violations in the organization and conduct of control, in the provision of medical care in a medical organization.
How are control results recorded and used?
Answer. The reports on the results of the control carried out are provided by medical insurance organizations to the territorial CHI fund. The medical insurance organization and the territorial CHI fund keep records of control acts. Accounting documents can be registers of acts of medical and economic control, medical and economic examination and examination of the ILC. The results of control in the form of acts are transferred to the medical organization within 5 working days. Possible maintenance electronic document management between subjects of control using an electronic digital signature.
In the event that the act is delivered to a medical organization personally by a representative of an insurance medical organization / territorial CHI fund, a mark of receipt is put on all copies of the act, indicating the date and signature of the recipient. When sending an act by mail, the specified document is sent by registered mail (with the preparation of an inventory) with notification.
The act can be sent to a medical organization in electronic form if there are guarantees of its reliability (authenticity), protection from unauthorized access and distortion.
The head of a medical organization or a person replacing him considers the act within 15 working days from the date of its receipt.
If the medical organization agrees with the act and the measures applied to the medical organization, all copies of the acts are signed by the head of the medical organization, sealed, and one copy is sent to the medical insurance organization / territorial CHI fund.
If the medical organization disagrees with the act, the signed act is returned to the medical insurance organization with a protocol of disagreements.
The territorial CHI fund, based on the analysis of the activities of the subjects of control, develops proposals that contribute to improving the ILC and the efficiency of using CHI resources and informs the executive authority of the constituent entity of the Russian Federation in the field of healthcare and territorial body Federal Service for Supervision of Healthcare and Social Development.
In accordance with Article 31 of the Federal Law, the presentation of a claim or claim against a person who has caused harm to the health of the insured person in order to reimburse the costs of paying for medical care provided by an insurance medical organization is carried out on the basis of the results of the examination of the ILC, drawn up by the relevant act.
Is it necessary to inform the insured about the violations found in the provision of medical care under the territorial compulsory medical insurance program?
Answer. Yes need. In order to ensure the rights to receive affordable and high-quality medical care, insured persons are informed by medical organizations, medical insurance organizations, territorial compulsory medical insurance funds about revealed violations in the provision of medical care under the territorial compulsory medical insurance program, including the results of control. Work with citizens 'appeals in the Federal CHI Fund, territorial CHI funds and medical insurance organizations is carried out in accordance with the Federal Law of 02.05.2006 N 59-FZ "On the Procedure for Considering Appeals of Citizens of the Russian Federation" and other regulatory legal acts regulating the work with citizens' appeals ... When a complaint from the insured person or his representative about the provision of medical care of inadequate quality is received by an insurance medical organization or a territorial CHI fund, the results of the consideration of the complaint based on the results of the examination of the ILC are sent to him.
How can a medical organization appeal the conclusion of an insurance medical organization based on the results of control?
Answer. In accordance with Article 42 of the Federal Law, a medical organization has the right to appeal the conclusion of an insurance medical organization based on the results of control within 15 working days from the date of receipt of acts of an insurance medical organization by sending a claim to the territorial CHI fund according to the recommended model.
The claim is made in writing and sent along with the necessary materials to the territorial fund of the CHI. The medical organization is obliged to submit to the territorial CHI fund: a) substantiation of the claim; b) a list of questions for each contested case; c) materials of internal and departmental control of the ILC in a medical organization.
The territorial CHI fund, within 30 working days from the date of receipt of the claim, considers the documents received from the medical organization and organizes repeated medical and economic control, medical and economic examination and examination of the ILC, which, in accordance with Part 4 of Article 42 of the Federal Law, are formalized by the decision of the territorial fund.
The decision of the territorial CHI fund, recognizing the correctness of the medical organization, is the basis for the cancellation (change) of the decision on non-payment, incomplete payment of medical care and / or on the payment of a fine by the medical organization for failure to provide, untimely provision or provision of medical care of inadequate quality based on the results of primary medical and economic expertise and / or expertise of the ILC.
The territorial CHI fund sends the decision based on the results of the re-examination to the medical insurance organization and to the medical organization that has sent a claim to the territorial CHI fund.
Changes in funding based on the results of consideration of disputed cases are carried out by an insurance medical organization no later than 30 working days (during the period of final settlement with a medical organization for the reporting period).
If the medical organization disagrees with the decision of the territorial fund, it has the right to appeal this decision in court.
Who and how can carry out the medical and economic examination and examination of the ILC?
Answer. In accordance with Part 5 of Article 40 of the Federal Law, a medical and economic examination is carried out by an expert who is a doctor with at least five years of experience in the medical specialty and has undergone appropriate training in expert activities in the field of compulsory medical insurance.
The main tasks of a specialist-expert are:
a) control of the compliance of the provided medical care with the terms of the contract for the provision and payment of medical care under the compulsory medical insurance by establishing the correspondence of the actual terms of medical care, the volumes of medical services provided for payment to the records in the primary medical and accounting documentation of the medical organization;
b) participation in organizing and conducting an examination of the ILC and ensuring the guarantees of the rights of insured persons to receive medical care of adequate quality.
The main functions of a specialist-expert are:
a) selective control of the volume of medical care for insured events by comparing actual data on the medical services provided to the insured person with the procedures for providing medical care and standards of medical care;
b) selection of cases for the ILC examination and justification of the need for it, preparation of the documentation necessary for the ILC expert to conduct the ILC examination;
c) preparation of materials for the methodological framework used for the examination of the ILC (procedures for the provision of medical care and standards of medical care, clinical protocols, guidelines, etc.);
d) generalization, analysis of the conclusions prepared by an expert of the ILC, participation in the preparation of an act of the established form or preparation of an act of the established form;
e) preparation of proposals for filing claims or claims against a medical organization for compensation for harm caused to insured persons and sanctions applied to a medical organization;
f) familiarization of the management of the medical organization with the results of the medical and economic examination and the examination of the ILC;
g) generalization and analysis of control results, preparation of proposals for the implementation of targeted and thematic medical and economic examinations and examinations of the ILC;
h) assessment of the satisfaction of the insured persons with the organization, conditions and quality of the medical care provided.
The examination of the ILC in accordance with part 7 of Article 40 of the Federal Law is carried out by an ILC expert who is a specialist doctor with a higher professional education, a certificate of accreditation of a specialist or a certificate of a specialist, work experience in the relevant medical specialty for at least 10 years and has been trained in expert activities in the field of compulsory medical insurance, included in the territorial register of experts of the ILC.
The ILC expert conducts the ILC examination in his main medical specialty, determined by a diploma, a certificate of accreditation of a specialist or a certificate of a specialist.
During the examination of the ILC, the ILC expert has the right to maintain anonymity / confidentiality.
The main task of the ILC expert is to conduct an examination of the ILC in order to identify defects in medical care, including assessing the correctness of the choice of a medical organization, the degree of achievement of the planned result, establishing causal relationships of the identified defects in medical care, drawing up an expert opinion and recommendations for improving the ILC in compulsory health insurance.
The ILC expert is not involved in the ILC examination in a medical organization with which he has an employment or other contractual relationship, and is obliged to refuse to conduct the ILC examination in cases when the patient is (was) his relative or a patient in whose treatment the ILC expert took part ...
ILC expert during the ILC examination:
a) uses medical documents containing a description of the treatment and diagnostic process, if necessary, examines patients;
b) provides information on the regulatory documents used (procedures for the provision of medical care and standards of medical care, clinical protocols, methodological recommendations) at the request of officials of the medical organization in which the examination of the ILC is carried out;
c) complies with the rules of medical ethics and deontology, maintains medical secrecy and ensures the safety of medical documents received for temporary use and their timely return to the organizer of the examination of the ILC or to a medical organization;
d) during the full-time examination, the ILC discusses with the attending physician and the management of the medical organization the preliminary results of the ILC examination.
The territorial register of the ILC experts contains information about the ILC experts who carry out the ILC examination as part of the control in the constituent entity of the Russian Federation, and is a segment of the unified ILC experts register.
The territorial register of ILC experts is maintained by the territorial CHI funds in accordance with clause 9 of part 7 of article 34 of the Federal Law on the basis of uniform organizational, methodological, software and technical principles.
Responsibility for violations in maintaining the territorial register of ILC experts lies with the director of the territorial CHI fund.
In accordance with clause 11 of part 8 of article 33 of the Federal Law, the OMS Federal Fund maintains a unified register of ILC experts, which is a set of electronic databases of territorial registers of ILC experts.
Problem Research Center
health and education
In accordance with the Federal Law of November 29, 2010 N 326-FZ "On compulsory health insurance in the Russian Federation" i order:
1. To approve the attached Procedure for organizing and monitoring the volumes, terms, quality and conditions for the provision of medical care for compulsory health insurance (hereinafter referred to as the Procedure).
2. The heads of territorial funds of compulsory medical insurance and medical insurance organizations shall use the attached Procedure when organizing and monitoring the volumes, terms, quality and conditions for the provision of medical care for compulsory medical insurance.
Chairman A. Yurin
The procedure for organizing and monitoring the volumes, terms, quality and conditions for the provision of medical care under compulsory health insurance
I. General provisions
1. This Procedure for organizing and monitoring the volume, timing, quality and conditions of providing medical care for compulsory health insurance (hereinafter referred to as the Procedure) has been developed in accordance with Federal Law of November 29, 2010 N 326-FZ "On Compulsory Health Insurance in the Russian Federation "(Collected Legislation of the Russian Federation, 06.12.2010, N 49, Art. 6422) and defines the rules and procedure for organizing and conducting by insurance medical organizations and compulsory medical insurance funds of control over the volumes, terms, quality and conditions for the provision of medical care by medical organizations in the amount and on the conditions established by the territorial compulsory health insurance program and the contract for the provision and payment of medical care for compulsory health insurance.
2. The purpose of this Procedure is to regulate measures aimed at the implementation of the rights of insured persons to receive free medical care in accordance with the territorial program of compulsory medical insurance and the contract for the provision and payment of medical care for compulsory medical insurance in volumes, terms and conditions, of proper quality in medical organizations participating in the implementation of compulsory health insurance programs.
II. Objectives of control of volumes, terms, quality and conditions of provision
medical assistance for compulsory health insurance
3. The control of the volume, timing, quality and conditions of the provision of medical care under compulsory health insurance (hereinafter - control) includes measures to verify the compliance of the medical care provided to the insured person with the terms of the contract for the provision and payment of medical care under compulsory health insurance, implemented through medical economic control, medico-economic examination and examination of the quality of medical care.
4. The object of control is the organization and provision of medical care for compulsory health insurance. The subjects of control are territorial compulsory medical insurance funds, medical insurance organizations, medical organizations entitled to carry out medical activities and are included in the register of medical organizations operating in the field of compulsory medical insurance.
5. Objectives of control:
5.1. ensuring free provision of medical care to the insured person in the amount and under the conditions established by the territorial compulsory medical insurance program;
5.2. protection of the rights of the insured person to receive free medical care in the amount and under the conditions established by the territorial compulsory health insurance program, of appropriate quality in medical organizations participating in the implementation of compulsory health insurance programs, in accordance with contracts for the provision and payment of medical care for compulsory health insurance ;
5.3. prevention of medical care defects resulting from the inadequacy of the medical care provided to the health status of the insured person; non-compliance and / or incorrect implementation of the procedures for the provision of medical care and / or standards of medical care, medical technologies by analyzing the most common violations based on the results of control and taking measures by the authorized bodies;
5.4. verification of the fulfillment by medical insurance organizations and medical organizations of their obligations to pay and provide free medical care to insured persons under compulsory medical insurance programs;
5.5. checking the fulfillment by medical insurance organizations of obligations to study the satisfaction of insured persons with the volume, availability and quality of medical care;
5.6. optimization of the cost of paying for medical care in the event of an insured event and reduction of insurance risks in compulsory health insurance.
6. Control is carried out by means of medical and economic control, medical and economic examination, examination of the quality of medical care.
III. Medical and economic control
7. Medical and economic control in accordance with part 3 of article 40 of the Federal Law of November 29, 2010 N 326-FZ "On Compulsory Medical Insurance in the Russian Federation" (hereinafter - the Federal Law) - establishing the compliance of information on the volume of medical care provided to insured persons on the basis of the registers of invoices submitted for payment by the medical organization to the terms of contracts for the provision and payment of medical care under compulsory medical insurance, the territorial compulsory medical insurance program, methods of payment for medical care and tariffs for payment of medical care.
8. Medical and economic control is carried out by specialists of medical insurance organizations and territorial compulsory medical insurance funds.
9. During medical and economic control, all cases of medical care are monitored for compulsory medical insurance in order to:
1) checking account registers for compliance with the established procedure for information exchange in the field of compulsory health insurance;
2) identification of the person insured by a specific medical insurance organization (payer);
3) checking the compliance of the provided medical care:
a) the territorial compulsory health insurance program;
b) the terms of the contract for the provision and payment of medical care for compulsory health insurance;
c) a valid license of a medical organization to carry out medical activities;
4) checking the validity of the application of tariffs for medical services, calculating their cost in accordance with the methodology for calculating tariffs for payment for medical care approved by the authorized federal executive body, methods of payment for medical care and tariffs for payment for medical care and an agreement for the provision and payment of medical care for compulsory health insurance;
5) establishing that the medical organization does not exceed the amount of medical care established by the decision of the commission for the development of a territorial compulsory medical insurance program, payable from compulsory medical insurance funds.
10. The violations identified in the account registers are reflected in the act of medical and economic control (Appendix 1 to this Procedure) with an indication of the amount of account reduction for each register entry containing information about medical care defects and / or violations in the provision of medical care.
In accordance with parts 9 and 10 of Article 40 of the Federal Law, the results of medical and economic control, drawn up by the relevant act in the form established by the Federal Fund for Compulsory Medical Insurance, are the basis for the application of measures provided for in Article 41 of the Federal Law, the terms of the contract for the provision and payment of medical care on compulsory medical insurance and a list of grounds for refusing to pay for medical care (reducing the payment for medical care) (Appendix 8 to this Procedure), and may also be the basis for a medical and economic examination; organization and examination of the quality of medical care; conducting repeated medical and economic control, repeated medical and economic expertise and expertise of the quality of medical care by the territorial compulsory medical insurance fund or by an insurance medical organization at the request of the territorial fund (except for control when making payments for medical care provided to insured persons outside the subject of the Russian Federation, for territory of which the compulsory health insurance policy was issued).
IV. Medical and economic expertise
11. Medical and economic examination in accordance with part 4 of article 40 of the Federal Law - establishing the correspondence of the actual terms of medical care, the volume of medical services presented for payment to the records in the primary medical documentation and accounting and reporting documents of the medical organization.
12. Medical and economic examination is carried out by a specialist expert (paragraph 78 of Section XIII of this Procedure).
13. Medical and economic expertise is carried out in the form of:
a) targeted medico-economic expertise;
b) planned medical and economic examination.
14. Targeted medical and economic examination is carried out in the following cases:
a) repeated visits for the same disease: within 30 days - in the provision of outpatient care, within 90 days - in case of repeated hospitalization;
b) diseases with an extended or shortened period of treatment by more than 50 percent of the established standard of medical care or average for all insured persons in the reporting period with a disease for which there is no approved standard of medical care;
c) receiving complaints from the insured person or his representative about the availability of medical care in a medical organization.
15. On the basis of the conducted medical and economic control, a planned medical and economic examination is carried out according to invoices submitted for payment within a month after the provision of medical assistance to the insured person under compulsory medical insurance, in other cases it can be carried out within a year after the presentation of invoices for payment.
16. When carrying out a planned medical and economic examination, the following are assessed:
a) the nature, frequency and causes of violations of the rights of insured persons to receive medical care under compulsory health insurance in the amount, terms, quality and conditions established by the contract for the provision and payment of medical care under compulsory health insurance;
b) the volume of medical care provided by the medical organization and its compliance with the amount established by the decision of the commission for the development of the territorial compulsory health insurance program to be paid from the funds of compulsory health insurance;
c) the frequency and nature of violations by a medical organization of the procedure for forming account registers.
17. The volume of inspections during a planned medical and economic examination of the number of bills accepted for payment in cases of providing medical care for compulsory health insurance is determined by the contract for the provision and payment of medical care for compulsory health insurance and is not less than:
8% - inpatient medical care;
8% - medical care provided in the day hospital;
0.8% - outpatient and polyclinic medical care.
If within a month the number of defects in medical care and / or violations in the provision of medical care exceeds 30 percent of the number of cases of medical care for which a medical and economic examination was carried out, in the next month the volume of checks from the number of bills accepted for payment in cases the provision of medical care should be increased by at least 2 times compared to the previous month.
18. With regard to a certain set of cases of medical care, selected according to thematic criteria (for example, the frequency and types of postoperative complications, duration of treatment, the cost of medical services), a planned thematic medical and economic expertise.
19. Based on the results of the medical and economic examination, the expert expert draws up an act of the medical and economic examination (Appendix 2 to this Procedure) in two copies: one is transferred to the medical organization, one copy remains in the medical insurance organization / territorial compulsory medical insurance fund.
In accordance with part 9 of Article 40 of the Federal Law, the results of a medical and economic examination, drawn up by an appropriate act in the form established by the Federal Fund for Compulsory Medical Insurance, are the basis for applying to a medical organization the measures provided for in Article 41 of the Federal Law, the terms of an agreement for the provision and payment of medical assistance for compulsory health insurance and a list of grounds for refusing to pay for medical care (reducing payment for medical care) (Appendix 8 to this Procedure), and may also be the basis for an examination of the quality of medical care.
V. Examination of quality
medical care
20. In accordance with Part 6 of Article 40 of the Federal Law, the examination of the quality of medical care is the identification of violations in the provision of medical care, including the assessment of the correctness of the choice of medical technology, the degree of achievement of the planned result and the establishment of cause-and-effect relationships of the identified defects in the provision of medical care.
21. The examination of the quality of medical care is carried out by checking the compliance of the medical care provided to the insured person with the contract for the provision and payment of medical care under compulsory health insurance, the procedures for the provision of medical care and the standards of medical care, established clinical practice.
22. The examination of the quality of medical care is carried out by an expert of the quality of medical care included in the territorial register of experts on the quality of medical care (paragraph 81 of Section XIII of this Procedure) on behalf of the territorial fund of compulsory medical insurance or an insurance medical organization.
23. Expertise of the quality of medical care is carried out in the form of:
a) targeted expertise of the quality of medical care;
b) planned examination of the quality of medical care.
24. Targeted examination of the quality of medical care is carried out within a month after the provision of the insured event (medical services) for payment, except for the cases determined by the current legislation and the cases set forth in subparagraph "e" of paragraph 25 of this section.
25. Targeted examination of the quality of medical care is carried out in the following cases:
a) receiving complaints from the insured person or his representative about the availability and quality of medical care in a medical organization;
b) the need to confirm the volume and quality of medical care in cases selected during medical and economic control and medical and economic examination;
c) deaths in the provision of medical care;
d) nosocomial infection and complications of the disease;
e) primary disability of people of working age and children;
f) repeated justified treatment for the same disease: within 30 days - in the provision of outpatient care, within 90 days - in case of repeated hospitalization;
g) diseases with an extended or shortened period of treatment by more than 50 percent of the established standard of medical care or average for all insured persons in the reporting period with a disease for which there is no approved standard of medical care.
26. When conducting a targeted examination of the quality of medical care in cases selected based on the results of a targeted medical and economic examination, the general terms for conducting a targeted examination of the quality of medical care may increase up to six months from the date of the invoice for payment.
When conducting a targeted examination of the quality of medical care in cases of repeated admission (hospitalization) for the same disease, the established terms are calculated from the moment the invoice containing information on re-admission (hospitalization) is submitted for payment.
The timing of the targeted examination of the quality of medical care from the date of submission of the invoice for payment is not limited in cases of complaints from insured persons or their representatives, deaths, nosocomial infection and complications of diseases, primary disability of people of working age and children.
27. Conducting a targeted examination of the quality of medical care in the event of complaints from insured persons or their representatives does not depend on the time that has passed since the provision of medical care and is carried out in accordance with the Federal Law of May 2, 2006 N 59-FZ "On the Procedure for Considering Citizens' Appeals Of the Russian Federation "and other regulatory legal acts regulating the work with citizens' appeals.
28. The number of targeted examinations of the quality of medical care is determined by the number of cases requiring it to be carried out on the grounds specified in this Procedure.
29. A planned examination of the quality of medical care is carried out in order to assess the conformity of the volumes, terms, quality and conditions for the provision of medical care to groups of insured persons, divided by age, disease or group of diseases, stage of medical care and other signs, conditions stipulated by the contract for the provision and payment medical assistance for compulsory health insurance.
30. The scope of a routine examination of the quality of medical care is determined by the contract for the provision and payment of medical care for compulsory health insurance and is not less than:
in the hospital - 5% of the number of completed treatment cases;
day hospital - 3% of the number of completed treatment cases;
in the provision of outpatient care - 0.5% of the number of completed treatment cases based on the results of medical and economic control.
31. Routine examination of the quality of medical care is carried out in cases of medical care under compulsory health insurance, selected:
a) by random sampling;
b) on a thematically homogeneous set of cases.
32. A planned examination of the quality of medical care by a random sampling method is carried out to assess the nature, frequency and causes of violations of the rights of insured persons to timely receive medical care in the volume and quality established by the territorial compulsory medical insurance program, including those caused by improper implementation of medical technologies that led to a deterioration in health the insured person, additional risk of adverse consequences for his health, non-optimal spending of the resources of the medical organization, dissatisfaction with the medical care of the insured persons.
33. A planned thematic examination of the quality of medical care is carried out in relation to a certain set of cases of medical care provided under compulsory health insurance, selected according to thematic criteria in each medical organization or group of medical organizations providing medical care under compulsory medical insurance of one type or under the same conditions.
The choice of topics is carried out on the basis of the performance indicators of medical organizations, their structural divisions and specialized areas of activity:
a) hospital mortality, the incidence of postoperative complications, primary disability of people of working age and children, the frequency of readmission, the average duration of treatment, the cost of medical services and other indicators;
b) the results of internal and departmental quality control of medical care.
34. The planned thematic examination of the quality of medical care is aimed at solving the following tasks:
a) identification, establishment of the nature and causes of typical (repetitive, systematic) errors in the treatment and diagnostic process;
b) comparison of the quality of medical care provided to groups of insured persons, divided by age, sex and other characteristics.
35. A planned examination of the quality of medical care is carried out in each medical organization providing medical care under compulsory medical insurance, at least once during a calendar year, within the timeframes determined by the inspection plan (paragraph 51 of Section VII of this Procedure).
36. The examination of the quality of medical care can be carried out during the period of rendering medical assistance to the insured person (hereinafter - the full-time examination of the quality of medical care), including upon the request of the insured person or his representative. The main goal of full-time examination of the quality of medical care is to prevent and / or minimize the negative impact on the patient's health status of medical care defects.
An expert of the quality of medical care, with notifying the administration of a medical organization, can conduct a bypass of the units of a medical organization in order to control the conditions for the provision of medical care, prepare materials for an expert opinion, and also consult an insured person.
When consulting, the applied insured person is informed about his state of health, the degree of compliance of the provided medical care with the procedures for the provision of medical care and standards of medical care, the contract for the provision and payment of medical care for compulsory medical insurance with an explanation of his rights in accordance with the legislation of the Russian Federation.
37. The expert of the quality of medical care, who carried out the examination of the quality of medical care, draws up an expert opinion containing a description of the conduct and results of the examination of the quality of medical care, on the basis of which an act of examination of the quality of medical care is drawn up.
In accordance with parts 9 and 10 of Article 40 of the Federal Law, the results of the examination of the quality of medical care, drawn up by the relevant act in the form established by the Federal Fund for Compulsory Medical Insurance (Appendices 5, 6 to this Procedure), are the basis for applying the measures provided for by Article to a medical organization. 41 of the Federal Law, the terms of the contract for the provision and payment of medical care for compulsory medical insurance and a list of grounds for refusing to pay for medical care (reducing the payment for medical care) (Appendix 8 to this Procedure).
Based on the acts of examination of the quality of medical care, the authorized bodies are taking measures to improve the quality of medical care.
Vi. Procedure for implementation by the territorial fund
compulsory health insurance control over activities
health insurance organizations
38. The Territorial Compulsory Medical Insurance Fund, on the basis of Part 11 of Article 40 of the Federal Law, exercises control over the activities of medical insurance organizations by organizing control of the volumes, terms, quality and conditions for the provision of medical care, conducts medical and economic control, medical and economic examination, examination of the quality of medical help, including repeated.
39. Repeated medical and economic examination or examination of the quality of medical care (hereinafter referred to as re-examination) is a medical and economic examination conducted by another expert-expert or another expert of the quality of medical care examination of the quality of medical care in order to verify the validity and reliability of conclusions on previously adopted conclusions made a specialist-expert or an expert on the quality of medical care, who initially conducted a medical and economic examination or an examination of the quality of medical care.
A repeated examination of the quality of medical care can be carried out in parallel or sequentially with the first by the same method, but by a different expert on the quality of medical care.
40. The objectives of the re-examination are:
a) verification of the validity and reliability of the conclusion of a specialist expert or an expert on the quality of medical care who primarily conducted a medical and economic examination or an examination of the quality of medical care;
b) control of the activities of individual experts / experts on the quality of medical care.
41. Re-examination is carried out in the following cases:
a) the territorial fund of compulsory medical insurance conducts a documentary check of the organization of compulsory medical insurance by an insurance medical organization;
b) identification of violations in the organization of control by the medical insurance organization;
c) groundlessness and / or unreliability of the conclusion of the expert of the quality of medical care who carried out the examination of the quality of medical care;
d) receipt of a claim from a medical organization that has not been settled with an insurance medical organization (clause 73 of Section XI of this Procedure).
42. The territorial compulsory medical insurance fund notifies the medical insurance organization and the medical organization about the re-examination no later than 5 working days before the start of work.
To conduct a re-examination to the territorial compulsory health insurance fund, within 5 working days after receiving a relevant request, an insurance medical organization and a medical organization must provide:
medical insurance organization - copies of acts of medical and economic control, medical and economic examination and examination of the quality of medical care necessary for the re-examination;
medical organization - medical, accounting and reporting and other documentation, if necessary, the results of internal and departmental quality control of medical care, including that carried out by the health management body.
43. The number of cases subject to re-examination is at least 20% of all examinations for the corresponding period of time.
44. The territorial fund of compulsory medical insurance sends the results of the re-examination drawn up by the act (Appendix 7 to this Procedure) to the insurance medical organization and the medical organization no later than 20 working days after the end of the inspection. An insurance medical organization and a medical organization are obliged to consider these acts within 20 working days from the date of their receipt.
45. An insurance medical organization and a medical organization, in the absence of agreement with the results of the re-examination, shall send a signed act with a protocol of disagreements to the territorial fund of compulsory medical insurance no later than 10 working days from the date of receipt of the act.
The territorial compulsory health insurance fund, within 30 working days from the date of receipt, considers the act with the protocol of disagreements with the involvement of interested parties.
46. \u200b\u200bIn accordance with part 14 of article 38 of the Federal Law, the territorial compulsory medical insurance fund, in the event of violations of contractual obligations by an insurance medical organization, when reimbursing it for medical care costs, reduces payments by the amount of identified violations or unfulfilled contractual obligations.
The list of sanctions for violations of contractual obligations is established by an agreement on the financial support of compulsory health insurance, concluded between the territorial fund of compulsory health insurance and an insurance medical organization.
In accordance with this agreement, in the event of violations in the activities of an insurance medical organization, the territorial compulsory medical insurance fund uses the measures applied to the medical insurance organization in accordance with Part 13 of Article 38 of the Federal Law and the agreement on financial support of compulsory medical insurance or recognizes those applied by the medical insurance organization to the medical organization the measures are unreasonable.
47. The territorial fund of compulsory medical insurance, upon detecting violations in the organization and carrying out a medical and economic examination and / or examination of the quality of medical care, sends a claim to an insurance medical organization, which contains information about the control over the activities of an insurance medical organization:
a) the name of the commission of the territorial compulsory health insurance fund;
b) the date (period) of the inspection of the medical insurance organization;
c) the composition of the commission of the territorial compulsory medical insurance fund;
d) regulatory legal acts, which are the basis for monitoring the activities of an insurance medical organization for organizing and conducting control and the reasons for conducting control;
e) facts of improper fulfillment by the medical insurance organization of contractual obligations to organize and conduct control, indicating the acts of re-examination;
f) the measure of liability of the medical insurance organization for the violations identified;
g) attachments (copies of re-examination acts, etc.).
The claim is signed by the director of the territorial compulsory health insurance fund.
Execution of the claim is carried out within 30 working days from the date of its receipt by the medical insurance organization, about which the territorial compulsory medical insurance fund is informed.
48. If the territorial fund of compulsory medical insurance reveals during the re-examination of violations missed by the medical insurance organization during the medical and economic examination or examination of the quality of medical care, the medical insurance organization loses the right to use the measures applied to the medical organization for a timely undetected medical defect. assistance and / or disruption in the provision of medical care.
49. The medical organization returns the funds in the amount determined by the re-examination act to the budget of the territorial compulsory health insurance fund.
50. The Territorial Compulsory Health Insurance Fund analyzes the applications of insured persons, their representatives and other subjects of compulsory health insurance based on the results of control carried out by an insurance medical organization.
Vii. Interaction of subjects of control
51. The Territorial Compulsory Medical Insurance Fund coordinates the interaction of subjects of control on the territory of a constituent entity of the Russian Federation, carries out organizational and methodological work to ensure the functioning of control and protection of the rights of insured persons, coordinates the plans for the activities of medical insurance organizations in terms of organizing and conducting control, including plans inspections by medical insurance organizations of medical organizations providing medical care under contracts for the provision and payment of medical care under compulsory medical insurance.
52. When carrying out a medical and economic examination and examination of the quality of medical care, a medical organization provides specialists-experts and experts on the quality of medical care within 5 working days after receiving a request, medical, accounting and reporting and other documentation, if necessary, the results of internal and departmental quality control medical care.
53. In accordance with part 8 of Article 40 of the Federal Law, a medical organization has no right to prevent specialist experts and experts of the quality of medical care from accessing the materials necessary for conducting a medical and economic examination, examination of the quality of medical care and is obliged to provide the requested information.
54. Employees participating in the control are responsible for the disclosure of confidential information of limited access in accordance with the legislation of the Russian Federation.
55. On the basis of Article 42 of the Federal Law, the resolution of controversial and conflict issues arising in the course of control between a medical organization and an insurance medical organization is carried out by the territorial compulsory medical insurance fund.
The commission informs the interested parties and the executive authority of the constituent entity of the Russian Federation in the field of healthcare on the results of resolving controversial and conflict issues, on violations in the organization and conduct of control, in the provision of medical care in a medical organization.
VIII. Accounting and use
control results
56. Reports on the results of the control carried out are provided by medical insurance organizations to the territorial fund of compulsory medical insurance.
The medical insurance organization and the territorial compulsory medical insurance fund keep records of control acts.
Accounting documents can be registers of acts of medical and economic control (Appendix 2 to this Procedure), medical and economic expertise and expertise of the quality of medical care.
The results of control in the form of acts are transferred to the medical organization within 5 working days.
It is possible to conduct electronic document circulation between subjects of control using an electronic digital signature.
57. In the event that the act is delivered to a medical organization personally by a representative of an insurance medical organization / territorial fund of compulsory medical insurance, a mark of receipt is put on all copies of the act, indicating the date and signature of the recipient. When sending an act by mail, the specified document is sent by registered mail (with the preparation of an inventory) with notification.
The act can be sent to a medical organization in electronic form if there are guarantees of its reliability (authenticity), protection from unauthorized access and distortion.
58. The head of a medical organization or a person replacing him, considers the act within 15 working days from the date of its receipt.
If the medical organization agrees with the act and the measures applied to the medical organization, all copies of the acts are signed by the head of the medical organization, stamped, and one copy is sent to the medical insurance organization / territorial compulsory health insurance fund.
If the medical organization disagrees with the act, the signed act is returned to the medical insurance organization with a protocol of disagreements.
59. The territorial fund of compulsory medical insurance, based on the analysis of the activities of the subjects of control, develops proposals that contribute to improving the quality of medical care and the efficiency of using the resources of compulsory medical insurance and informs the executive authority of the constituent entity of the Russian Federation in the field of health care and the territorial body of the Federal Service for Surveillance in Healthcare and social development.
60. In accordance with Article 31 of the Federal Law, a claim or a claim against a person who has caused harm to the health of the insured person in order to reimburse the costs of payment for medical care provided by an insurance medical organization is based on the results of the examination of the quality of medical care, drawn up by the relevant act.
IX. The procedure for informing insured persons about revealed violations in the provision of medical care
according to the territorial compulsory health insurance program
61. In order to ensure the right to receive affordable and high-quality medical care, insured persons are informed by medical organizations, medical insurance organizations, territorial compulsory medical insurance funds about violations in the provision of medical care under the territorial compulsory medical insurance program, including the results of control.
62. Work with citizens' appeals in the Federal Compulsory Medical Insurance Fund, territorial compulsory medical insurance funds and medical insurance organizations is carried out in accordance with Federal Law of May 2, 2006 N 59-FZ "On the Procedure for Considering Appeals of Citizens of the Russian Federation" and other regulatory legal acts regulating the work with citizens' appeals.
63. When a complaint of the insured person or his representative for the provision of medical care of inadequate quality is received by an insurance medical organization or a territorial fund of compulsory medical insurance, the results of the consideration of the complaint based on the examination of the quality of medical care are sent to him.
64. In medical insurance organizations organizing the service of representatives of medical insurance organizations for the implementation in medical organizations participating in the implementation of compulsory health insurance programs, work to protect the rights and legitimate interests of insured persons, representatives of medical insurance organizations take part in the preparation and placement of information materials on protection of the rights of insured persons and the results of control, as well as provide insured persons receiving medical assistance in medical organizations with information and explanatory materials on their rights.
X. Procedure for the application of sanctions
to a medical organization for violations identified during control
65. On the basis of Part 1 of Article 41 of the Federal Law, the amount not payable based on the results of medico-economic control, medico-economic examination, examination of the quality of medical care is withheld from the amount of funds provided for payment of medical care provided by medical organizations, or is subject to refund to an insurance medical organization in accordance with the contract for the provision and payment of medical care for compulsory medical insurance, a list of grounds for refusing to pay for medical care or reducing the payment for medical care in accordance with this Procedure.
66. The result of the control in accordance with the contract for the provision and payment of medical care under compulsory health insurance and the list of grounds for refusing to pay for medical care (reducing the payment for medical care) are:
a) non-payment or reduction of payment for medical care in the form of:
exclusion of an item from the register of accounts payable for the volume of medical care;
decrease in the amounts presented for payment as a percentage of the cost of medical care provided for insured event;
return of unpaid amounts to an insurance medical organization;
b) payment of fines by a medical organization for failure to provide, untimely provision or provision of medical care of inadequate quality (for an insured event in which defects in medical care and / or violations in the provision of medical care were identified).
67. Non-payment or reduction of payment for medical care and payment of fines by a medical organization in accordance with subparagraph b) of paragraph 66 of this section, depending on the type of identified defects in medical care and / or violations in the provision of medical care, may be applied separately or simultaneously.
68. If violations of contractual obligations in relation to the volume, timing, quality and conditions of the provision of medical care are revealed, the medical insurance organization does not partially or fully reimburse the costs of the medical organization for the provision of medical care, reducing subsequent payments on the bills of the medical organization for the amount of identified defects in medical care and / or irregularities in the provision of medical care or requires the return of amounts to an insurance medical organization.
The amount that is not payable based on the results of the control is withheld from the amount of funds provided for payment of medical care provided by a medical organization, or is subject to return to an insurance medical organization in accordance with an agreement for the provision and payment of medical care for compulsory medical insurance.
69. For failure to provide, untimely provision, or provision of medical care of inadequate quality under an agreement for the provision and payment of medical care under compulsory health insurance, a medical organization pays a medical insurance organization a fine in the amount established under the said contract and in accordance with the list of grounds for refusal (reduction ) payment for medical care (Appendix 8 to this Procedure).
70. If there are two or more grounds for refusing to pay for medical care or reducing payment for medical care in the same case of rendering medical care, one is applied to the medical organization - the most significant ground entailing a larger amount of non-payment or refusal to pay. The summation of the amount of incomplete payment for medical services for one insured event is not made.
71. Failure to pay or incomplete payment of medical care, as well as the payment of fines by a medical organization for failure to provide, untimely provision or provision of medical care of inadequate quality does not exempt the medical organization from reimbursing the insured person for harm caused by the fault of the medical organization in the manner prescribed by the legislation of the Russian Federation.
72. Funds received as a result of the application of sanctions to a medical organization for violations revealed during the control are spent in accordance with the Federal Law.
XI. Appeal
medical organization conclusion of an insurance medical organization
based on control results
73. In accordance with Article 42 of the Federal Law, a medical organization has the right to appeal the conclusion of an insurance medical organization based on the results of control within 15 working days from the date of receipt of acts of an insurance medical organization by sending a claim to the territorial fund of compulsory medical insurance according to the recommended model (Appendix 9 to this Order).
The claim is made in writing and sent along with the necessary materials to the territorial compulsory health insurance fund. The medical organization is obliged to provide to the territorial compulsory health insurance fund:
a) substantiation of the claim;
b) a list of questions for each contested case;
c) materials of internal and departmental quality control of medical care in a medical organization.
74. The territorial fund of compulsory medical insurance, within 30 working days from the date of receipt of the claim, considers the documents received from the medical organization and organizes repeated medical and economic control, medical and economic examination and examination of the quality of medical care, which, in accordance with Part 4 of Article 42 of the Federal of the law are formalized by the decision of the territorial fund.
75. The decision of the territorial compulsory health insurance fund, recognizing the correctness of the medical organization, is the basis for canceling (changing) the decision on non-payment, incomplete payment of medical care and / or on the payment of a fine by the medical organization for failure to provide, untimely provision or provision of medical care of inadequate quality based on the results primary medical and economic examination and / or examination of the quality of medical care.
Changes in funding based on the results of consideration of disputed cases are carried out by an insurance medical organization no later than 30 working days (during the period of final settlement with a medical organization for the reporting period).
76. If the medical organization disagrees with the decision of the territorial fund, it has the right to appeal against this decision in court.
XII. Organization by the territorial fund of compulsory health insurance of control in the implementation of settlements
for medical assistance provided to insured persons outside the constituent entity of the Russian Federation,
in the territory of which the compulsory health insurance policy was issued
77. The organization by the territorial compulsory medical insurance fund of control when making payments for medical care provided to insured persons outside the constituent entity of the Russian Federation, on the territory of which the compulsory medical insurance policy was issued, is carried out in accordance with sections III-V of this Procedure.
XIII. Workers,
carrying out medical and economic expertise and expertise of the quality of medical care
78. In accordance with Part 5 of Article 40 of the Federal Law, medical and economic expertise is carried out by a specialist expert who is a doctor with at least five years of work experience in the medical specialty and has undergone appropriate training in expert activities in the field of compulsory health insurance.
79. The main tasks of a specialist-expert are:
a) control of the compliance of the provided medical care with the terms of the contract for the provision and payment of medical care for compulsory medical insurance by establishing the correspondence of the actual terms of the provision of medical care, the volumes of medical services provided for payment to the records in the primary medical and accounting documentation of the medical organization;
b) participation in organizing and conducting an examination of the quality of medical care and ensuring guarantees of the rights of insured persons to receive medical care of appropriate quality.
80. The main functions of a specialist-expert are:
a) selective control of the volume of medical care for insured events by comparing actual data on the medical services provided to the insured person with the procedures for providing medical care and standards of medical care;
b) selection of cases for examination of the quality of medical care and justification of the need for its implementation, preparation of the documentation necessary for an expert of the quality of medical care to conduct an examination of the quality of medical care;
c) preparation of materials for the methodological base used for the examination of the quality of medical care (procedures for the provision of medical care and standards of medical care, clinical protocols, guidelines, etc.);
d) generalization, analysis of conclusions prepared by an expert on the quality of medical care, participation in the preparation of an act of the established form or preparation of an act of the established form;
e) preparation of proposals for filing claims or claims against a medical organization for compensation for harm caused to insured persons and sanctions applied to a medical organization;
f) familiarization of the management of a medical organization with the results of medical and economic expertise and expertise of the quality of medical care;
g) generalization and analysis of control results, preparation of proposals for the implementation of targeted and thematic medical and economic examinations and examinations of the quality of medical care;
h) assessment of the satisfaction of the insured persons with the organization, conditions and quality of the medical care provided.
81. Examination of the quality of medical care in accordance with part 7 of Article 40 of the Federal Law is carried out by an expert on the quality of medical care who is a specialist doctor with a higher professional education, a certificate of accreditation of a specialist or a certificate of a specialist, work experience in the relevant medical specialty for at least 10 years and trained in expert activities in the field of compulsory health insurance, included in the territorial register of experts on the quality of medical care (paragraph 84 of this section).
An expert on the quality of medical care conducts an examination of the quality of medical care in his main medical specialty, determined by a diploma, a certificate of accreditation of a specialist or a certificate of a specialist.
When conducting an examination of the quality of medical care, an expert of the quality of medical care has the right to maintain anonymity / confidentiality.
82. The main task of an expert of the quality of medical care is to conduct an examination of the quality of medical care in order to identify defects in medical care, including assessing the correctness of the choice of a medical organization, the degree of achievement of the planned result, establishing causal relationships of identified defects in medical care, drawing up an expert opinion and recommendations for improvement quality of medical care in compulsory health insurance.
An expert on the quality of medical care is not involved in the examination of the quality of medical care in a medical organization with which he has an employment or other contractual relationship, and is obliged to refuse to conduct an examination of the quality of medical care in cases where the patient is (was) his relative or patient, in the treatment of which a quality care expert was involved.
83. Expert of the quality of medical care during the examination of the quality of medical care:
a) uses medical documents containing a description of the treatment and diagnostic process, if necessary, examines patients;
b) provides information on the regulatory documents used (procedures for the provision of medical care and standards of medical care, clinical protocols, guidelines) at the request of officials of the medical organization in which the quality of medical care is being examined;
c) complies with the rules of medical ethics and deontology, maintains medical secrecy and ensures the safety of medical documents received for temporary use and their timely return to the organizer of the examination of the quality of medical care or to a medical organization;
d) discusses with the attending physician and the management of the medical organization the preliminary results of the examination of the quality of medical care.
84. The territorial register of experts on the quality of medical care contains information about experts of the quality of medical care who carry out expert examination of the quality of medical care within the framework of control in the constituent entity of the Russian Federation, and is a segment of the unified register of experts on the quality of medical care.
The territorial register of experts on the quality of medical care is maintained by the territorial compulsory medical insurance funds in accordance with clause 9 of part 7 of article 34 of the Federal Law on the basis of uniform organizational, methodological, programmatic and technical principles.
Responsibility for violations in maintaining the territorial register of experts on the quality of medical care is borne by the director of the territorial compulsory medical insurance fund.
In accordance with paragraph 11 of Part 8 of Article 33 of the Federal Law, the Federal Compulsory Medical Insurance Fund maintains a unified register of experts on the quality of medical care, which is a set of electronic databases of territorial registers of experts on the quality of medical care.
Healthcare of the Stavropol Territory has a developed network that provides the population with the provision of timely and high-quality medical care. To date, 130 medical organizations of various organizational and legal forms and forms of ownership function in the region's compulsory health insurance system.
The planning of the volume of medical care and the financial and economic substantiation of the size of the per capita standard of financial support for 2015 was carried out taking into account the standards for the volume of medical care by type, conditions and forms of medical care, in accordance with the Territorial program of state guarantees of free provision of medical care to citizens in the Stavropol Territory for 2015 and the planning period of 2016 and 2017, approved by the decree of the Government of the Stavropol Territory dated December 25, 2014 No. 542-p.

The results of the implementation of the Territorial Compulsory Health Insurance Program for the 1st half of 2015 have been summed up.
The planned volumes of medical care for the 1st half of 2015 amounted to 10 billion 581 million rubles in total for the region.
According to the types of institutions, planned financing was formed as follows:
regional medical organizations - 2 billion 177 million rubles or 21%;
city \u200b\u200bmedical organizations - 4 billion 974 million rubles or 47%;
central regional hospitals - 3 billion 430 million rubles or 32%.
The amount of invoices issued for payment according to the data of medical insurance organizations for the 1st half of 2015 amounted to 10 billion 956 million rubles or 104%.
The amount of invoices accepted for payment according to the CMO data for the 1st half of 2015 as a whole amounted to: 10 billion 287 million rubles in total, or 97%:
regional medical organizations - 2 billion 033 million rubles or 93%;
city \u200b\u200bmedical organizations - 4 billion 783 million rubles or 96%;
central regional hospitals - 3 billion 471 million rubles, or 101%.

In connection with the appeal of medical organizations on increasing the volume of medical care and financial support for 2015, the audit and analytical department of the TFOMS SK carried out analytical work on the results of the implementation in the 1st half of 2015 of the planned volumes of medical care in the Andropov Central District Hospital, Novoselitskaya Central District Hospital, Neftekum Central District Hospital, Krasnogvardeyskaya CRH, as well as all primary vascular departments of the region, based on information obtained during inspections, as well as information obtained from a database of personalized accounting. The purpose of the audit was to identify the main problems based on the results of the activities of medical organizations, which led to the lack of financial support in 2015.
A structural analysis of the economic losses of the above medical organizations due to non-payment of account registers based on the results of the TFOMS SK and medical insurance organizations of medical and economic control, medical and economic examination, and examination of the quality of medical care was carried out. The above economic losses are irreversible for most medical organizations due to expired re-invoicing.

The main causes of economic losses are:
ineffective planning of financial and economic activities;
defects in planning the volume of medical care;
cases of unjustified hospitalization;
defects in the preparation of primary medical documentation revealed during the examination;
violations in the registration of account registers;
the presence of interrupted cases of treatment;
irrational spending of compulsory medical insurance funds.
In general, in the region, the amount of non-payment of account registers by insurance companies amounted to 670 million rubles.

For example:
Izobilnenskaya Central District Hospital - according to the results of the first half of 2015, the total amount of non-payment of invoices for actually executed volumes amounted to 30 million 132 thousand rubles;
Children's Hospital of Filippsky - 27 million 493 thousand rubles;
Krasnogvardeyskaya Central District Hospital - non-payment, excluding re-issued volumes, amounted to 14 million 443 thousand rubles;
Neftekum CRH - the amount of non-payment for the first half of 2015 amounted to 16 million 122 thousand rubles;
Novoselitskaya Central District Hospital - according to the results of the first half of 2015, the total amount of non-payment amounted to 8 million 847 thousand rubles.

Despite the implementation of a number of measures aimed at structural transformations of the system for the provision of specialized medical care, the development of hospital-replacing technologies, the improvement of the provision of outpatient care to the population, a comparative analysis of the volume of medical care provided in inpatient conditions and day hospitals indicates that a rather significant amount of inpatient medical care.
At the same time, inpatient medical care consumes most of the financial resources. cHI systems... Therefore, a prerequisite for the effective development of the industry is not only the improvement of the structure of medical care provided to the population, but also the improvement of methods of payment for it using those of them that, by providing medical organizations with the necessary financial resources, will stimulate them to use modern medical technologies and improve treatment methods.
The 24-hour hospital in 2015 operates on 258 KSGs, the planned volumes were agreed upon jointly with the participation of heads of medical organizations, the Ministry of Health of the Territory and TFOMS SK at the conciliation commission on December 16, 2014. But despite this, the results of activities at the end of the first half of 2015 in the context of medical organizations show us that not all organizations provide medical care in accordance with the planned volumes, that is, there is ineffective planning in the context of DRGs and, as a result, economic losses and insufficiency financial security.

So, for the round-the-clock hospital in general, the implementation of the planned number of hospitalizations for 2015 in the first half of 2015 was 52%.
As a result of the structural analysis of the implementation of the planned volumes of medical care for 2015 in 68 medical organizations with a round-the-clock hospital, at the end of the first half of 2015, the following performance indicators are noted:
the full compliance of the planned volumetric indicators of medical care for 2015 with those fulfilled for the analyzed period in the round-the-clock hospital is demonstrated by 5 medical organizations, which is 7% of all that have a round-the-clock hospital in their structure: Apanasenkovskaya CRH, Trunovskaya CRH, GKB No. 3 in Stavropol, Regional Oncological Dispensary and Regional Uroandrological Center;
the fulfillment of the annual plan is less than 50% registered in 25 medical organizations or 37%;
excess of planned indicators by more than 50% is observed in 38 medical organizations or 56%.

A structural analysis was carried out in the context of clinical and statistical groups for the effectiveness of planning, execution of the state assignment both in terms of volume indicators of activity and financial performance of the plan in the context of medical insurance organizations.
The structural analysis of the performed volumes of medical care in the round-the-clock hospital in the context of the DRC showed the following. Fulfillment of the annual plan for hospitalizations as a whole in the region was less than 50% for 138 DRCs, with a plan of 216,215 cases for the amount of 4 billion 525 million rubles. actual execution amounted to 75 thousand 357 cases in the amount of 1 billion 380 million rubles. Estimated economic losses for the first half of 2015 amounted to 3 billion 144 million rubles, which indicates ineffective planning of the volume of medical care.

First of all, the following DRGs draw attention to themselves:
“Bowel operations (level 3)”, in which only 78 cases were performed against the planned 1447 cases, which is 5%;
"Diabetes mellitus without complications, adults" - with a plan of 4,856 cases, only 408 or 8% were completed;
"Infections of the skin and subcutaneous tissue" - with the plan of 3,657 cases, only 299 or 8% were completed;
“Cerebral infarction, treatment with thrombolytic therapy” - with a plan of 870 cases, only 58 or 7% were completed;
“Unstable angina pectoris, myocardial infarction, pulmonary embolism, treatment with thrombolytic therapy” - with a plan of 1,380 cases, only 98 or 7% were completed;
"Angina pectoris (except unstable), chronic ischemic heart disease, coronary angiography was performed" with a plan of 1,024 cases, 112 or 11% were completed.
First of all, this concerns the PSO and RSC, and such a percentage of the planned volume of medical care for clinical and statistical groups of diseases of the circulatory system, which are one of the main causes of premature mortality and disability of the population, is of concern.

It is noted that the plan for hospitalizations is more than 50% for 106 DRGs, with the percentage of implementation varying from 51 to 3638%.
A significant overfulfillment of the plan was noted for the following DRGs:
“Operations on the organ of hearing, paranasal sinuses and upper respiratory tract (cost level 2) with a plan of 813 cases, performed 2315 or 284%. When analyzing the overfulfillment of the volumetric indicators for this DRG in the context of medical institutions, it is noted that 151 cases are planned in the regional children's clinical hospital in Stavropol, 555 cases or 367% completed, in the city children's clinical hospital named after Filippsky in Stavropol - the above operations were not planned, completed - 396.
The maximum excess of the planned indicators was noted for the CGS "Angioedema, anaphylactic shock" - with a plan of 8 cases, 291 or 3637% were completed. The overfulfillment of volumes for this CGS was registered in almost all MOs.
The excess of financing due to overfulfillment of the planned target according to the data of the CGS amounted to 1 billion 880 million rubles.
For example, due to ineffective planning and the lack of adjustments to the planned target at the end of the first half of 2015 for a round-the-clock hospital, the estimated economic losses due to failure to fulfill the planned volumes are:
In the Andropov Central District Hospital, due to non-fulfillment of the planned volumes of 64 DRGs, the estimated economic losses amounted to 9 million 450 thousand rubles;
in the Novoselitskaya Central District Hospital - 8 million 214 thousand rubles;
In the Neftekum Central Regional Hospital - 3 million 502 thousand rubles.
At the same time, in these medical organizations, for numerous DRGs, there is a significant excess of the annual plan, both in terms of volume and financial indicators.
So, in the Neftekum Central Regional Hospital, the fulfillment of the annual plan by more than 50% was revealed for 60 KSG. With the planned cost of 56 million 679 thousand rubles per year, 39 million 848 thousand rubles were actually paid, which is 70.3% of the annual plan;
in Novoselitskaya Central District Hospital there is an excess of the planned volume of 35 KSG. The planned cost for 2015 for the specified KSG is 11 million 564 thousand rubles, in fact, payment was made in the amount of 13 million 354 thousand rubles, that is, the annual plan for 6 months in terms of financial indicators was fulfilled by 115.5%;
in the Andropov Central District Hospital, the planned volumes of 2015 for 42 KSG were exceeded. The planned cost of the said KSG is 30 million 816 thousand rubles, the actual payment was 21 million 508 thousand rubles, that is, the annual plan in terms of financial indicators was fulfilled by 69.8%.
Based on the analysis carried out, it can be concluded that the adjustment of the planned target for the volume of medical care in the 24-hour hospital by medical organizations is not made and, accordingly, the planned funding as a whole is distorted.

Day care activities
Despite the implementation of a number of measures aimed at structural transformations of the system of specialized medical care, the development of hospital-replacing technologies, the situation is as follows. Planned indicators for the provision of medical care in day hospitals of the Stavropol Territory at the end of the 1st half of 2015 were fulfilled by 47%.

Compliance of the performed volumes of medical care with the planned ones was noted only in 4 medical organizations: "Department Hospital of the Russian Railways, Mineralnye Vody", "Arzgir Central District Hospital", "City Polyclinic No. 1" of Nevinnomyssk, "Nevinnomyssk Medical and Rehabilitation Center".
Completion of less than 50% - in 52 municipalities, of which 16 CRHs, 31 city hospitals and 5 regional institutions;
Over 50% exceeded the approved indicators - 34 medical organizations, of which 9 are central regional hospitals, 20 city municipalities and 5 regional ones.

A comparative analysis of the performance of day hospitals in the context of DRGs revealed the fulfillment of the plan for hospitalizations of less than 50% for 71 DRGs with a plan of 97,469 cases for the amount of 1 billion 203 million rubles. actual execution amounted to 37,329 cases in the amount of RUB 484 million. Estimated economic losses for the 1st half of 2015 amounted to 718 million rubles, which indicates ineffective planning of the volume of medical care.
In addition, a vivid example of ineffective planning for a day hospital in terms of a significant overfulfillment of the planned target is the volume of assistance provided for 19 DRCs, where the percentage of fulfillment varies from 100 to 4200%.

The most indicative are the execution of volumes for the following CGS:
"Diabetes mellitus with complications, adults", planned 102 cases per year, completed 273 or 277%.
"Diseases of the pancreas", 287 cases planned per year, 571 or 199% completed.
"Pneumonia, pleurisy, other pleural diseases", 96 cases planned per year, 124 or 129% completed.
"Chemotherapy for other malignant neoplasms of lymphoid and hematopoietic tissues, adults", 13 cases planned, 94 or 723% completed.
"Liver disease, level 2", 2 cases planned, 84 or 4200% completed !!
And there are many such examples!
At the same time, the plan for the day hospital is adjusted by medical organizations in isolated cases. Using the example of the same medical organizations, we note the facts of ineffective planning in day hospitals, and as a result, the discrepancy between the actually performed volumes of medical care in the day hospital in the context of the DRG and the financial execution of the state assignment for 2015:
in the Andropov Central District Hospital, the financial performance of the day hospital plan at the end of the first half of 2015 due to non-performance of volumes (according to personalized accounting data) amounted to 38%. The estimated economic losses due to failure to fulfill the planned volumes amounted to 1 million 679 thousand rubles at the end of the first half of 2015;
in the Krasnogvardeyskaya Central Regional Hospital for the day hospital as a whole, the plan was fulfilled by 60%, which in the total amount of actually paid account registers is 15 million 942 thousand rubles. The planned cost of all DRGs for 2015 for day hospital is 26 million 044 thousand rubles. Proceeding from this, the excess of financing at the end of the 1st half of 2015 due to the overfulfillment of volumes amounted to 2 million 920 thousand rubles;
in the Neftekum CRH for day hospital as a whole, according to the results of the first half of 2015, the plan was fulfilled by 57%, which in the total amount of actually paid account registers is 11,139 thousand rubles. The planned cost of all day hospital KSGs is 10 million 166 thousand rubles. Based on this, the excess of financing due to the overfulfillment of volumes amounted to 973 thousand rubles;
The ineffective planning of the DRG and the implementation of the volumes of medical care for the unplanned DRGs was revealed, which led, accordingly, to non-compliance with the planned volumes of financial support for 2015.
In the "Neftekum CRH", the implementation of the volume of medical care for unplanned DRCs was identified in 21 DRCs, where 127 patients were treated for a total of 1 million 842 thousand rubles. Medical insurance organizations have requested medical records to check the validity of hospitalizations in a 24-hour hospital. The results of the expert examination upon completion of the work will be communicated to the interested parties.
And such planning defects are inherent in almost all medical organizations!

We carried out a structural analysis of the 24-hour hospital interruptions. As a result, it was revealed that in general in the Stavropol Territory in the system of compulsory medical insurance, economic losses due to interrupted cases of treatment for the first half of 2015 amounted to 328 million rubles;
Economic losses by type of institution were as follows:
Central regional hospitals - 82 million rubles;
In medical organizations located in the cities of the region - 198 million rubles;
Regional medical organizations - 48 million rubles.
The main reasons for aborted cases are:
death of the patient, which is 10% of the total number of interrupted cases of treatment,
transfer to another medical organization - 25%,
discharge for reasons beyond the control of the medical organization - 65%.
A structural analysis of interrupted cases of treatment of patients in a round-the-clock hospital showed that the proportion of patients discharged for reasons beyond the control of the medical organization in the first half of 2015 was 65%.
Patients discharged for reasons beyond the control of the medical organization are divided into the following categories:
treatment was interrupted at the initiative of the patient - 46%;
treatment was interrupted at the initiative of a medical organization - 9%;
treatment interrupted due to transfer to a day hospital - 2%;
treatment was interrupted due to transfer to another profile of the bed fund - 20%;
unauthorized patient leaving - 23%.
To reduce the volume of economic losses due to preventable causes, medical organizations should pay attention to the main problems of interrupted cases of treatment:
discharge at the initiative of the patient;
unauthorized patient leaving;
non-compliance with the prescribed regimen, drug therapy;
technical errors in the formation of registers-accounts: incorrect filling of the fields of registers-accounts, technical errors made during the implementation of the software product in medical organizations.
The TFOMS SK recommends to the heads of medical organizations to take measures to eliminate the preventable causes of interrupted cases. To reduce the number of interrupted cases due to reasons of “discharge at the initiative of the patient” and “unauthorized care”, it is necessary to conduct explanatory work with patients, since in most cases, premature discharge of patients leads to repeated hospitalizations. We also propose to strengthen control over patients of round-the-clock and day hospitals by the middle and junior medical personnel to eliminate such reasons for discharge as violation of the regime and unauthorized care.
To eliminate technical errors when issuing registers-invoices, TFOMS SK invites you to bring the conditions for issuing registers-invoices in medical organizations in accordance with the requirements of the Tariff Agreement and pay particular attention to Article 39 "Rules for payment of interrupted cases of treatment in inpatient and day hospital conditions" and table 10 "List of CGS, payment for ultra-short cases of medical care attributed to which is carried out at the tariff of CGS regardless of the actual stay of the patient", since most of the interrupted cases in the account registers refer to this list.

The analysis of the functioning of a single information resource (or EIR263), through which data exchange is carried out when organizing information support of insured persons in the context of medical organizations and bed fund profiles, for the reliability and timely updating of information about the functioning of the bed fund in a round-the-clock hospital. As a result of the analysis, it was revealed that the share of unjustified emergency hospitalization in the total number of patients admitted to a 24-hour hospital varies from 20% to 30%, depending on the level and profile of medical organizations.
Most medical organizations do not correct the data in a timely manner or do not enter data on the discharge of patients into the EIR263 software resource at all.
Starting from July 2014 and during the current year, TFOMS SK has repeatedly sent recommendatory and organizational letters to the heads of the MO on the functioning of the EIR263 software resource, but despite this, the defects in the organization of the work of the MO operators in the software package are not eliminated.
The contact information of the Ministry of Defense is not filled out in 50% of organizations, despite comments and explanations, for example, in the Petrovskaya Central District Hospital, Kochubeevskaya Central District Hospital, Emergency Hospital in Stavropol, Arzgirskaya Central District Hospital, Grachevskaya Central District Hospital, Andropovskaya Central District Hospital.
Data on the discharge of patients on time are not entered in the Stavropol Emergency Hospital (3587 patients were not discharged), Novoselitskaya Central District Hospital (874 patients were not discharged), the Regional Perinatal Center (625 patients were not discharged), while the number of patients exceeds the number of beds required to complete the state assignment.

Monitoring of the implementation of the planned volume indicators of the territorial compulsory medical insurance program for the 1st half of 2015 was carried out in the context of all areas of the outpatient service.
Outpatient and polyclinic medical care is provided in 117 medical organizations of the region operating in the compulsory medical insurance system, including 99 medical organizations and 18 dental clinics.
In general, the volume of visits in the region was performed by 102% of the plan for the 1st half of 2015, including 94% - due to illness, 124% - for preventive purposes and 70% - for emergency medical care.
Including services for the child population, the volume of visits in the region was 110% of the plan for the 1st half of 2015 (including 95% due to illness, 133% for preventive purposes and 66% for emergency medical care).

The fulfillment of the planned volume indicators by the medical organizations of the region in the context of appeals due to the disease amounted to 97% of the plan of the year in the region, including child population - 96%.
In a significant number of medical organizations, non-fulfillment of the plan for appeals due to illness is due to the overfulfillment of planned volume indicators for visits with a preventive purpose.
Most medical organizations receive treatment for a disease by calculation, which is unacceptable. We would like to draw your attention to the fact that it is necessary to keep a separate record of "complaints about diseases" and not to allow distortions of the actual volumes by type of visits.
The fulfillment of planned volume indicators by medical organizations of the region in the context of visits with a preventive purpose amounted to 124% in the whole region, and 133% in the children's population. The main reasons for such an increase in preventive visits are: disorganized accounting of visits, inconsistency between planned volumes and actually executed, incorrect application of tariffs and, as a consequence, distortion of the planned target.

In order to increase the efficiency of the timely identification of risk factors for diseases and the organization of their correction, as well as early diagnosis of diseases, which to the greatest extent determine the disability and mortality of the population of the region, medical organizations of the region conduct medical examinations of the population.
Clinical examination of the adult population in 2015 is planned in the Stavropol Territory in the amount of 500 thousand 112 people. As a result of the activities of 49 medical organizations, 254 thousand 280 people underwent medical examination, which is 51% of the annual plan.
Fulfillment of the annual plan below 30% was noted in the "City Polyclinic No. 1" in Pyatigorsk, "Ipatovskaya Central Regional Hospital", "City Polyclinic" in Essentuki.

Preventive examinations of the adult population of the region for 2015 are planned in the amount of 90 thousand 970 people. In the first half of 2015, 30 thousand 322 people underwent preventive medical examinations, which is 33% in the region. Low percentage performance was noted in the "City Polyclinic No. 1" of Pyatigorsk, "Andropovskaya Central Regional Hospital", "Ipatovskaya Central Regional Hospital".
Clinical examination of orphans staying in inpatient institutions, and children in difficult life situations, as well as orphans and children left without parental care, including those adopted (adopted), taken under guardianship (guardianship), in a foster care or foster care family in 2015 in the Stavropol Territory is subject to the plan of 6 thousand 966 people. For the past 6 months of 2015, 2 thousand 745 cases were accepted for payment on the conducted medical examination, which is 39% of the annual plan.
Fulfillment of the annual plan 0% !!! noted in "Aleksandrovskaya Central Regional Hospital", "Budennovskaya Central Regional Hospital", "Neftekum Central Regional Hospital", "Novoselitskaya Central Regional Hospital". The main reason, according to the Ministry of Defense, is planning the volume of medical examination for the autumn period in connection with the beginning of the school year. For preventive medical examinations of minors in 2015, 213 thousand 575 people are planned. For the first half of 2015, 92 thousand 944 cases were accepted for preventive medical examinations of minors, which is 44%.
Fulfillment of the annual plan 0% !!! noted in the "Neftekum CRH" and in the "Novoselitskaya CRH" due to the lack of specialists.
For the periodical medical examinations of minors in 2015, 119 thousand 872 people are planned. In the first half of 2015, 23,074 people underwent periodic medical examinations of minors, which is 19% in the whole region.
Fulfillment of the annual plan 0% !!! noted in the "Neftekum Central Regional Hospital", "Novoselitskaya Central District Hospital", "Petrovsky Central District Hospital", "Blagodarny Central District Hospital", "Andropov Central District Hospital".
The fulfillment of planned volume indicators by medical organizations of the region in the context of visits to emergency medical care amounted to 70% in general in the region, including 66% in the child population.
The main reason for the failure to fulfill the plan for emergency medical care is due to the fact that medical institutions of the region often charge for the case of providing medical care in an emergency form to patients as a case of a single visit by a patient to a medical organization in connection with an illness, or include it in the rate of treatment and thereby choosing more high payment for the finished case.

For the ambulance in the Stavropol Territory, in accordance with the approved assignment, the planned volume indicators for 2015 were fulfilled for the first half of 2015 by 50%.

With the plan of 814 thousand 674 calls, the fact was 411 thousand 075 calls. Out of 411 thousand calls, 392 thousand or 96% of emergency calls were made, 19 thousand or 4% of urgent calls.

Performance financial indicators 2015 according to the results of the first half of the year amounted to 48%. With the plan of 1 billion 339 million rubles, the fact was formed in the amount of 642 million rubles.
In the structure of emergency calls, cardiovascular diseases make up the highest percentage of the total number of calls.

In order to monitor compliance with the terms, procedures and standards for the provision of medical care to patients with acute cerebrovascular accidents and acute coronary syndrome in primary vascular departments, the use of compulsory medical insurance by medical organizations, unscheduled thematic inspections of all primary vascular departments of the Stavropol Territory were carried out.

The checks revealed the following problems and violations. The bed fund of the PSO in most organizations does not correspond to the amount of assistance actually provided in connection with the attachment to the PSO in accordance with the order of the Ministry of Health of the SK dated July 08, 2013 No. 01-05 / 764 of municipalities and urban districts and medical assistance in the PSO is provided on the attached non-estimated bunks. Which leads to overfulfillment of the approved volumes.
The implementation of the planned volumes of medical care at the end of the first half of 2015 in the PSO was as follows:
"Regional Center of the UHMWP No. 1" - 57%;
"GKB" of Pyatigorsk - 55%;
GKB No. 3, Stavropol - 43%;
Essentuki Central City Hospital - 43%;
Kislovodsk Central City Hospital - 95%;
"City Hospital" in Nevinnomyssk - 68%;
"Petrovskaya Central District Hospital" - 30%.
There is an extremely low implementation of the planned indicators of thrombolytic therapy in all medical organizations that have a PSO in their structure. At the same time, the purchase of the necessary drugs is made in full for 2015, as a result of which there is a high probability of expiration of the shelf life of expensive thrombolytics.
As a result of the structural analysis carried out on interrupted cases of treatment in the PSO, it showed that the economic losses of the PSO amounted to 39 million rubles in the first half of 2015. The main reasons for the formation of interrupted treatment cases are:
deaths - 625 cases; transfer to other medical organizations - 280 cases; discharge for reasons beyond the control of the medical organization - 187 cases.
The highest volume of economic losses due to interrupted cases of treatment in the PSO in the first half of 2015 was noted in:
Essentuki Central City Hospital - 6 million rubles;
Kislovodsk Central City Hospital - 4 million rubles;
"GKB" of Pyatigorsk - 7 million rubles;
GKB No. 3, Stavropol - 11 million rubles.
As a result of checking the causes of the interrupted cases, it was revealed that interrupted cases of treatment in the PSO were billed for payment in the registries of treatment with the outcome - recovery, but with deviations in the patient's treatment time from the approved average duration by 2-3 days, which could be billed as completed cases treatment. These facts are noted in all medical organizations that have a PSO in their structure.
The account registers do not include codes of services provided to patients, including the code for thrombolytic therapy, which significantly affects the cost of a treatment case in one direction or another.
This problem has been identified in all medical organizations of the Stavropol Territory. Based on this, there is a violation in terms of the correctness and validity of the application of tariffs and the formation of the cost of cases of medical care.
Comparative analysis of primary medical documentation and information in account registers showed the following violations.
Cases of treatment included in the DRC "Cerebral infarction with thrombolysis" and "Unstable angina pectoris, myocardial infarction, pulmonary embolism with thrombolysis" are exhibited and paid for as completed cases with 100% payment, and the medical history records a transfer to the RSC after thrombolytic therapy on the first day from the onset of the disease. In fact, these are interrupted cases of treatment according to the terms of the tariff agreement. These violations were noted in the "Essentuki Central City Hospital", "GKB" in Pyatigorsk.
Defects in the design of primary medical documentation were identified, which made it difficult to conduct an examination of the quality of medical care in terms of determining contraindications to thrombolytic therapy, incorrect filling of checklists for deciding the possibility of thrombolysis.
The facts were revealed that the treatment cases included in the DRC "Brain infarction with thrombolysis" were billed, where thrombolytic therapy was not actually carried out, thrombolytic drugs were not used in the treatment of patients, the patients were treated not in the PSO, but in the neurological department of the hospital.
For all verified case histories, estimates of the actual costs incurred per PSO patient were requested. The analysis showed that in most cases the costs of diagnostics and treatment exceed the funds received, and the actual average duration of treatment has significant deviations from the approved one and ranges from 3 to 25 days.
In this regard, the commission for the development of a territorial compulsory health insurance program approved for all levels of medical organizations, regardless of the duration of the patient's actual stay, an interrupted case of medical care related to the DRC specified in table 11.1 of the tariff agreement must be presented for payment with a coefficient of 0.8 ...

Based on the results of the inspections, the TFOMS SK proposes, in order to reduce the mortality rate in medical organizations and reduce the mortality rate of the population of the Stavropol Territory from circulatory diseases, which are the main causes of premature mortality and disability, to bring the quality of medical care to patients of the PSO in accordance with the approved procedures and standards of care.

TFOMS SK conducted an analysis of the cash and actual execution of financial support of medical organizations under the territorial CHI program, which revealed ineffective planning of financial and economic activities.
In addition, I would like to note that improper planning and organization of the treatment process, as well as non-compliance with the volume of the state order for the provision of medical care by type of expense, based on the approved plan of financial and economic activities, leads to the formation of accounts payable.
In general, the region's accounts payable as of 01.01.2015 amounted to 204 million rubles and for 6 months of the current year increased by 463 million rubles in comparison with the beginning of the year. or 3.3 times, which as of 01.07.2015 amounted to 667 million rubles or 227%.
So, in the Regional Perinatal Center accounts payable as of 01.07.2015 amounted to 13.9 million rubles, or 155% since the beginning of the year.
Accounts payable in Novoselitskaya Central Regional Hospital as of 01.07.2015 amounted to 6.5 million rubles, or 46.3% since the beginning of the year.
In the Neftekum Central Regional Hospital, accounts payable as of 01.07.2015 amounted to 25.7 million rubles, or 134.2% from the beginning of the year.
In the Andropov Central Regional Hospital, accounts payable as of 01.07.2015 amounted to 12.9 million rubles, or 174.5% from the beginning of the year.

According to the monitoring data for the 1st half of 2015, the target indicators for the ratio of the average salary of doctors, middle and junior medical personnel in the Stavropol Territory as a whole have been met.
Formation of reports on wages by order of FFOMS No. 65 dated 26.03.2013 continues in the current year. Wages are under special control in the MHIF. As part of the implementation of this order, inspections of medical organizations continue on the facts of a decrease in the average salary of medical personnel compared to the previous year and compliance with the target indicators for the ratio of the average salary by category of personnel.

Also, a comparative analysis of the average salary approved according to the "Roadmap" for 2015, and monitoring data by categories of personnel in the CHI system for the 1st half of 2015 was carried out.
The analysis showed that in some medical organizations, when the indicators for some categories of employees are exceeded, for other specialists, the average salary, approved by the Road Map for 2015, is not met.

At the same time, in some medical organizations, there is an overfulfillment of the planned salary indicators approved by the Roadmap for 2015.
For example, the analysis carried out in GBUZ IC "Novoselitskaya Central District Hospital" of the volume of medical care under the territorial program of compulsory health insurance revealed irrational planning of financial and economic activities. At the end of the 1st half of 2015, salaries exceeded the planned indicators according to the roadmap for doctors by 26.8%, for nurses by 8.2% and junior by 5.0%. Thus, in GBUZ IC "Novoselitskaya CRH" the actual payroll with charges for the first half of 2015 exceeded the indicators approved by the "road map" of the Moscow region by 4 million 240 thousand rubles, or 10%.

In the course of the audit of the Neftekum CRH, when analyzing the cash and actual execution of financial support for the volume of medical care under the territorial compulsory medical insurance program for the 1st half of 2015, irrational planning of financial and economic activities was revealed, in particular, the diversion of funds from the expenditure item "wages with payroll charges" on the item "medicines and dressings" in the absence of savings in financial resources provided for labor costs. At the same time, the salary in the first half of 2015 exceeded the targets for the state assignment by 10%, and according to the roadmap by 5%. In the absence of financial support, the volume of purchases of medicines unjustifiably increased, as a result, as of July 1, 2015, accounts payable amounted to 17.6 million rubles.
Thus, the existing accounts payable and the existing balance of medicines in the warehouse and in the departments will not allow to ensure a high-quality treatment process in accordance with the standards of medical care by the end of 2015. Taking into account the ongoing monitoring of wages, the shortcomings revealed during the inspections, it is advisable to strictly follow the indicators provided for by the "road map".
Please note that the assessment of the activities of medical organizations depends on the quality of the reports provided regarding wages, analytical tables, analysis of indicators. Based on the reporting of TFOMS SK, analytical reports are provided to the regional government, the Ministry of Healthcare of the SK, the MHIF. The analysis of the indicators of the reporting forms is used by the regulatory authorities during inspections.

TFOMS SK and CMO carried out a sociological monitoring of citizens' satisfaction with the provided medical services. The study of citizens' satisfaction with the quality of medical care in the CHI system is a socially significant indicator characterizing the activity of the CHI system as a whole.
In the first half of 2015, 33 thousand people took part in the survey.Sociological monitoring showed that the number of people satisfied with the provided medical care decreased by 2%, the number of dissatisfied people increased by 1%, the share of respondents partially satisfied with the medical care provided increased, and the number of respondents who did not decide on attitude to medical care.
The population of the Stavropol Territory is more satisfied with hospital-substituting medical care, least of all respondents are satisfied with the organization of the provision of outpatient medical care, including the low availability of specialist consultations, laboratory and instrumental studies. Higher level of satisfaction with the organization of work of children's hospitals
Dear Colleagues!
Based on the results of the analysis, we can see that there is a clear tendency to exceed the planned volumes for a round-the-clock hospital, outpatient and polyclinic care. I would like to remind you that an Agreement has been concluded between the Ministry of Health of the Russian Federation, FFOMS and the Government of the UK, which clearly sets out the standards for the volume of medical care provided to residents of the UK. Financial support for the list of insured events, types and conditions for the provision of medical care is carried out subject to the fulfillment of the requirements established by the basic and territorial CHI Program. Responsibility for the implementation of all the terms of the Agreement, as you understand, lies not only with the Government of the UK, the Ministry of Health, and the Foundation, but also with the direct executors implementing the territorial Program, that is, with you, dear leaders. The excess of the state assignment will be clearly monitored by both the Fund and medical insurance organizations. Corresponding measures will be taken on the revealed violations.
In conclusion, I want to say that work is already underway to plan the state assignment for 2016. Taking into account the analysis of the activities of medical organizations for the first half of 2015, I ask you to take into account all the problems noted in the report and I want to direct the heads of medical institutions to more rational and effective planning of medical care, financial and economic activities, in order to avoid economic losses in 2016 and, as a result, insufficient financial support for medical organizations.
Ministries
health care of the Kaliningrad region
and TFOMS of the Kaliningrad region
dated March 15, 2019 N 167/102
Regulations
monitoring and control over the implementation of the volume of medical care and financial resources established by the decision of the Commission for the development of a territorial program of compulsory medical insurance of the Kaliningrad region
Scroll
abbreviations used in the Regulation
|
Reduction |
Definition |
|
VMP |
High-tech medical care |
|
Commission |
Commission for the development of the Territorial MHI Program |
|
MO |
Medical organization participating in the implementation of the TP OMS |
|
IEC |
Medical and economic control |
|
IEE |
Medical and economic expertise |
|
OMS |
Mandatory health insurance |
|
Reporting period (month) |
The period (month) in which medical assistance was provided to the insured persons, incl. previously started treatment cases completed |
|
Working group |
Working group under the Commission for the development of TP for OMS |
|
Medical care register |
Electronic register of personalized accounting of information about medical care provided to insured persons |
|
CMO |
Medical insurance organization |
|
TP OMS |
Territorial program of compulsory medical insurance of the Kaliningrad region |
|
TFOMS |
Territorial fund of compulsory medical insurance of the Kaliningrad region |
|
EKMP |
Examination of the quality of medical care |
|
GBUZ KO |
State budgetary institutions health care of the Kaliningrad region |
I. Basic provisions
1. This Regulation was developed in accordance with the Federal Law of November 29, 2010 N 326-FZ "On compulsory medical insurance in the Russian Federation", by order of the Ministry of Health and Social Development of Russia dated February 28, 2011 N 158n "On approval of the Rules of compulsory medical insurance", by order of the Ministry of Health Of the Russian Federation dated 24.12.2012 N 1355n "On approval of the form of a standard agreement for the provision and payment of medical care for compulsory medical insurance", by order of the Ministry of Health and Social Development of Russia dated 09.09.2011 N 1030n "On approval of the form of a model agreement on financial support of compulsory medical insurance", by order Federal Compulsory Medical Insurance Fund dated 01.12.2010 N 230 "On approval of the Procedure for organizing and conducting control of volumes, terms, quality and conditions for the provision of medical care for compulsory medical insurance."
2. The Regulation establishes uniform organizational and methodological principles for monitoring and controlling the volume of medical care and financial resources within the framework of the TP of the CHI.
3. Basic principles of monitoring and control:
1) monitoring and control of the implementation of the volumes established by the decision of the Commission is carried out on an accrual basis from the beginning of the year, taking into account the implementation of quarterly and annual plans in the context of the conditions for the provision of medical care and in the context of medical institutions;
2) the monthly plan is conventionally considered 1/3 of the volume established by the decision of the Commission for the Ministry of Defense for the quarter. The implementation of the plan is calculated on an accrual basis for the reporting period from the planned volumes, conditionally calculated for this period, based on the actually accepted medical care volumes for payment, taking into account the IEC results (except for the IEC results for the code of reason for refusing to pay for medical care 5.3.2 " Presentation for payment of cases of medical care in excess of the distributed volume of medical care, established by the decision of the Commission for the development of a territorial program ");
3) the planned volumes for which monitoring and control is carried out are the volumes approved by the last decision of the Commission;
4) monitoring and control are carried out in relation to the volumes of medical care and financial resources established by the decision of the Commission, including the volumes of separately planned types of medical care (medical services):
In general, for the TP of the compulsory medical insurance, for all municipalities for each condition for the provision of medical care: outpatient care (the number of visits in total, including for preventive and other purposes (including individual events), the number of emergency visits, the number of visits and visits regarding the disease ; ambulance (calls); inpatient care, including VMP (hospitalizations, bed-days); in a day hospital (cases of treatment, patient-days);
By profiles, groups and types of PMF in accordance with the distribution of PMF volumes between MOs, approved by the Commission;
For certain types of primary health care and primary specialized medical care on an outpatient basis, which are not included in the per capita standard for financing outpatient care for attached persons (medical care provided in an emergency form, preventive measures, dental care, methods of renal replacement therapy, and other types approved by the decision of the Commission);
For certain types and profiles of specialized medical care in the context of clinical and statistical groups of diseases and separately paid services (medical rehabilitation, methods of renal replacement therapy, in vitro fertilization, chemotherapy of malignant neoplasms, the use of genetically engineered drugs, surgery on the organs of vision (level 5, 6 in the context of a certain list of services), complex treatment with the use of immunoglobulin preparations) and other clinical and statistical groups of diseases approved by the decision of the Commission);
5) the amount of medical care provided (including certain types of medical care and medical services), established for the year with a quarterly breakdown and reasonable subsequent adjustments, is subject to payment;
6) as part of the control of the volumes established by the Commission, the reception of registers for medical care provided, including VMP, other separately planned types of medical care (medical services), is carried out within the quarterly plan;
7) reception of registers of medical care in excess of the quarterly plan established by the Commission is carried out on the basis of applications of the Ministry of Defense, recognized by the Commission as reasonable, with subsequent adjustment of the quarterly and annual volumes of medical care, taking into account the actual performance;
8) adjustment of the volume of medical care is carried out:
In general, for the TP of the CHI within the volumes established for the corresponding year under the terms of provision;
By redistributing volumes between medical institutions, taking into account the reorganization of medical institutions, the closure and opening of departments, the consumption of medical care by insured persons, including due to the routing of patient flows in a three-level system of medical care;
For MO by changing the annual plan or without changing the annual plan with quarterly redistribution in accordance with the application, to change the established volumes;
In case of recognition of a justified request by the Ministry of Defense for quarterly redistribution when receiving registers of medical care in excess of the quarterly plan established by the Commission, the adjustment is carried out by increasing the quarterly plans specified in the application and reducing the plan for subsequent quarters without increasing the annual plan;
For the HMP by redistributing the volume of medical care within the TP of the CHI;
For preventive measures by redistributing the volume of medical care between medical institutions within the framework of the annual volumes established for a specific measure;
In terms of the volume of certain expensive medical technologies through redistribution between medical institutions within the established annual volumes for a specific medical technology;
9) the reasons for the justified excess of the planned volumes / justified application for changing the established volumes of medical care may be:
An increase in the number and / or change in the gender and age composition of insured persons who have chosen this MO for the provision of primary health care or sent to this MO in accordance with the routing, confirmed by acts of reconciliation with the CMO, which led to an increase in the consumption of medical care by insured persons;
Changes in the routing of patient flows, including due to the reorganization of medical facilities, changes in the structure of a medical organization (opening of new departments, medical appointments, an increase in bed capacity), confirmed by relevant regulations, which led to an increase in the consumption of medical care by insured persons;
Outbreaks of infectious diseases (excess of the incidence rate in comparison with the average annual indicators), confirmed by Rospotrebnadzor data, emergencies, man-made disasters, natural disasters, etc., other reasons leading to a significant increase in the volume of emergency and / or emergency medical care;
10) in other cases, when the responsibility of the Ministry of Defense to manage the hospitalization process in round-the-clock and day hospitals is violated in the form of regulation in the context of forms of medical care (emergency, planned), which is expressed in excess of the volume of planned medical care, the provision of applications by the Ministry of Defense for changing the established volumes medical care is unreasonable.
When providing outpatient medical care in the context of appeals, visits, emergency medical care and other conditions for the provision of medical care, which is expressed in the excess of the volumes of the listed medical activities (for example, visits), the provision of applications by the Ministry of Defense for changing the established volumes of medical care is unreasonable.
11) within the framework of monitoring the volume of medical care and financial resources, measures are being taken, provided for by the order of the FFOMS dated 01.12.2010 N 230 "On approval of the Procedure for organizing and monitoring the volume, timing, quality and conditions of providing medical care for compulsory medical insurance."
II. Medical organizations
4. Organize the provision of medical care in accordance with the Territorial program of state guarantees of free provision of medical care to citizens in the Kaliningrad region within the scope established by the decision of the Commission, in accordance with the contract for the provision and payment of medical care for compulsory medical insurance.
5. Carry out monitoring of the fulfilled volumes of medical care according to the terms of provision on a monthly cumulative basis from the beginning of the year.
6. Take measures to prevent exceeding the volume of medical care (according to the conditions of provision and certain types of medical care or medical services) established by the decision of the Commission for the relevant period, by regulating the priority for planned hospitalization, keeping logs of planned hospitalization, strengthening the role of the outpatient clinic, development of day hospitals, etc.
7. Analyze the performance indicators of medical institutions (the function of the medical position, the structure of visits, the structure of hospitalizations, the average bed occupancy, the duration of hospitalization, the proportion of hospitalized in a planned and urgent / emergency order, waiting time for planned hospitalization, the cost of a unit of medical care, etc. ) for the timely adoption of managerial decisions, including the redistribution of the volume of medical care between structural units, subject to agreement with the Ministry of Health of the Kaliningrad region.
8. Within 5 working days after making changes to the structure of the bed fund and day hospital places, this information is brought to the attention of the TFOMS and the medical center with the provision of the structure of the institution approved by the Ministry of Health of the Kaliningrad Region.
9. If there is a justified need to change the volume of medical care established by the decision of the Commission, form a single application in accordance with Appendix No. 1 to this Regulation and send it to:
1) the chairman of the commission for the development of a territorial compulsory health insurance program (Ministry of Health of the Kaliningrad Region);
2) the deputy chairman of the commission for the development of a territorial compulsory health insurance program (territorial compulsory health insurance fund).
10. The MO application for a change in the established volumes of medical care can be of two types: for a quarterly redistribution of volumes without changing the annual plan and for a change in the annual plan:
1) if there is a justified need to download the registers of medical care in excess of the previously established quarterly plan, the Ministry of Defense form an application for quarterly redistribution - within the established annual plan;
2) to increase the volume of medical care in excess of the established annual plan - in the case when overfulfillment of the quarterly plan will reasonably lead to an overfulfillment of the annual volume of medical care;
3) an application for changing volumes must be sent no later than 5 working days of the month following the reporting period. Copies of the necessary documents are attached to the application (orders on the reorganization of the medical institution, the redistribution of patient flows, on the opening / closing of departments, etc.). Applications submitted in violation of this procedure are not subject to consideration;
4) if the planned volumes of medical care are not fulfilled, an application for the quarterly redistribution of these volumes is not submitted, the redistribution of the unfulfilled medical care volumes, if necessary, is carried out by the Commission on the proposals of the Working Group.
11. The Ministry of Defense, which by the decision of the Commission established the volumes of VMP for the corresponding year:
1) take measures to prevent the excess of the volume of VMP by the types of VMP established by the decision of the Commission, by regulating the priority for planned hospitalization, maintaining priority logs for the provision of VMP;
2) enter information about the fact of the provision of high-tech medical care in the specialized information system of the Ministry of Health of the Russian Federation;
3) send to the Chairman of the Commission an application for changing the planned volumes of the VMP with justifications for making the changes.
12. Conclude an additional agreement on amending the contract for the provision and payment of medical care for compulsory health insurance with the health insurance company in accordance with the decision of the Commission.
III. Medical insurance organizations
13. On a monthly accrual basis from the beginning of the year, the Ministry of Health monitors the volumes of medical care and financial resources performed according to the terms of medical care.
14. Analyze the performance indicators of the established volumes and the reasons for excess / non-compliance with the volume of medical care and financial resources for all conditions of medical care.
15. Establish the validity of the reasons for exceeding / not fulfilling the volume of medical care, analyzing the structure of treated patients, the availability of referrals for planned hospitalization, the proportion of emergency / urgent hospitalizations, including for certain classes of diseases, the planned and actual duration of treatment, the indicator of operational activity, etc. measures taken by the head of the Ministry of Defense to regulate the priority for planned hospitalization, including for high-tech medical care, continuity in the work of hospitals, polyclinics, day hospitals.
16. Carry out MEE, EKMP, including face-to-face checks, in order to identify cases of unjustified hospitalizations (including repeated), non-core hospitalizations, as well as other violations of the procedures and standards of medical care, violations of primary medical documentation and the formation of account registers leading to unjustified excess of the established volumes of medical care.
17. By the decision of the Commission, if the fact of exceeding the volume of medical care established for the Ministry of Defense in general in the reporting period is recognized as unjustified, in accordance with the order of the MHIF dated 01.12.2010 N 230 "On approval of the Procedure for organizing and conducting control of volumes, terms, quality and conditions provision of medical care for compulsory health insurance "is carried out by the IEC, including repeated, in cases of medical care presented for payment by the MO in excess of the established amount:
1) the number of cases included by the HMO in the IEC act should not exceed the number of cases presented by the HMO to pay for this HMO in excess of the established planned volume;
2) if the excess of the established plan for a specific HMO is greater than the excess for the whole MO, then the number of cases included in the IEC act should not exceed the total number of cases of medical care presented by the MO for payment in excess of the plan.
18. According to the decision of the Commission on amending the distribution of medical care and / or the amount of financial resources between MOs under the TP, MHI conclude additional agreements to contracts for the provision and payment of medical care for compulsory health insurance with the MO.
IV. Ministry of Health of the Kaliningrad Region
19. Carries out work on the optimization and re-profiling of bed capacity in subordinate medical organizations in accordance with the standards and routing of patient flows, taking into account the level of medical care.
20. Informs the Working Group in advance about the planned reorganization of medical facilities, the closure / opening of departments and changes in patient routing.
21. Prepares materials for consideration at the meetings of the Working Group and the Commission within its competence.
22. Carries out monthly monitoring of the fulfillment of the planned volumes of the PMF by types of PMF and MO, as well as the analysis of requests from the Ministry of Defense for the redistribution of the established volumes of the PMF; proposals on the redistribution of the planned volumes of VMP by types of VMP, with justification, are sent to the Working Group.
23. With the involvement of the main freelance specialists of the Ministry of Health of the Kaliningrad region of the relevant profiles:
1) analyzes the execution of volumes for certain expensive medical technologies, established by the decision of the Commission, on a quarterly basis;
2) provides information on the validity of exceeding the volumes of certain expensive medical technologies in the context of medical facilities and sends to the Working Group proposals for additional loading of these volumes in excess of the quarterly plan and the redistribution of volumes between quarters and (or) medical facilities.
V. Territorial fund of compulsory medical insurance of the Kaliningrad region
24. On a monthly basis, on an accrual basis, monitors and analyzes the implementation of the volume of medical care and financial resources established by the decision of the Commission, in the context of MO and separately planned types of medical care (medical services).
25. Prepares materials for consideration at the meetings of the Working Group and the Commission.
26. By the decision of the Commission, it reallocates the volume of medical care and financial resources between the Ministry of Defense and the Medical Association.
27. Carries out control over the activities of health care organizations, including by organizing repeated control of the volumes, terms, quality and conditions for the provision of medical care under the compulsory medical insurance, in order to identify violations in the provision of medical care leading to an excess of the established volumes.
28. Analyzes the violations identified during the control of the volumes, terms, quality and conditions for the provision of medical care under compulsory medical insurance, as well as the structure of medical care in the MO, which exceeded the volumes of medical care and financial resources established by the Commission.
29. Informs the Ministry of Health of the Kaliningrad Region, as well as the Working Group about the violations revealed during the control (including repeated) of the volumes, terms, quality and conditions for the provision of medical care under the compulsory medical insurance.
30. Assess the amount of funding established by the decision of the Commission and the amounts actually presented for payment for compliance with the standards of financial costs per unit of medical care, established by the TP of the CHI.
31. Conducts an analysis of the planned and actual cost per unit of medical care in accordance with the Tariff Agreement on CHI to identify the reasons for the deviation of the actual cost indicators from the planned indicators.
32. Within 5 working days after the meeting of the Commission, informs interested parties about the decisions taken by the Commission by posting it on the official website of the TFOMI.
Vi. Working group under the Commission for the development of the territorial CHI program
33. Analyzes the implementation of the TP of the compulsory medical insurance under the conditions for the provision of medical care in the context of medical institutions, types of high-tech medical care, separately planned types of medical care (medical services).
34. Considers applications received from medical organizations included in the register in the current financial year.
35. Taking into account the proposals of the Ministry of Health of the Kaliningrad Region, TFOMS of the Kaliningrad Region, prepares a draft decision for consideration by the Commission:
1) on the validity of the Ministry of Defense's applications for the formation of additional registers of medical care in excess of the quarterly plan and the need to adjust the established volumes of medical care;
2) on the validity of the MO applications for changing the established volumes of medical care.
36. If necessary, at the meetings of the Working Group, hears representatives of the Ministry of Defense who have exceeded the volume of medical care established by the decision of the Commission.
37. Submits to the Commission for consideration proposals on the establishment / redistribution of the volume of medical care and financial resources between the Ministry of Defense as a whole, as well as proposals on the establishment / redistribution of volumes by types of HMP, separately planned types of medical care (medical services).
- Appendix N 1. Application of a medical organization to change the volume of medical care established by the decision of the commission for the development of a territorial compulsory medical insurance program